The impact of liver cancer continues to be felt on our community. Despite efforts to better understand and treat this disease, since the turn of the century, incidence rates of liver cancer have almost doubled and survival rates remain low.
Of the 1000-plus people in NSW who are diagnosed with liver cancer each year, sadly only one in five (or 21 per cent) will live beyond five years.
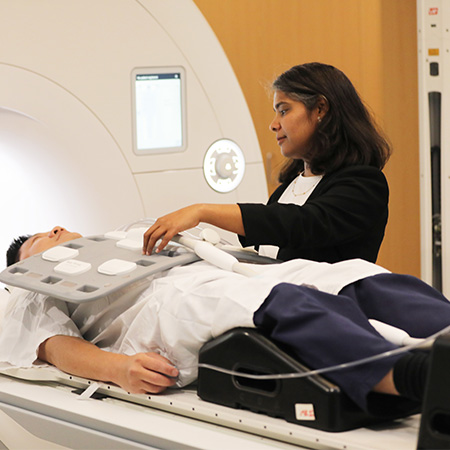
Dr Sirisha Tadimalla has experienced the devastation of liver cancer firsthand. In 2006, her mother lost her life to the disease at 50 years old. This has driven her to pursue a career in liver cancer research, using her expertise as a magnetic resonance imaging (MRI) physicist to make a difference for people facing a poor prognosis.
“My mother had no history of liver disease and lived a healthy lifestyle. Yet by the time she was diagnosed, the cancer was too advanced for treatment,” Dr Tadimalla said.
“That experience left a profound impact on me and has driven my commitment to improving outcomes for patients with poor-prognosis liver cancer.”
In 2023, Dr Tadimalla received an Early Career Fellowship from the Cancer Institute NSW to develop a new way to personalise liver cancer radiation treatment through MRI.
From limited treatment options to hope
Liver cancers often present late, when treatment options are limited and constrained by underlying liver disease such as cirrhosis.
An emerging treatment called stereotactic body radiation therapy (SBRT) is showing promising survival outcomes as it allows high doses of radiation to be delivered more precisely to the tumour. However, a significant amount of people with advanced liver cancer also have impaired liver function which affects treatment options and outcomes. For these people, they are either ineligible for the SBRT or are given reduced doses to preserve their remaining liver function. These low doses only slow disease progression and do not offer a cure.
Dr Tadimalla and her team are aiming to make SBRT safer and more effective for this vulnerable group of patients. They are using MRI to create images of the liver that show regions of high and low function, just like a rainfall map.
“My work uses MRI to generate spatial maps of liver function, showing which regions are healthy and which are impaired,” Dr Tadimalla explained.
“By identifying those regions, we can tailor the radiation treatment to the individual patient. High energy radiation beams needed to ensure the tumour receives a lethal dose of radiation can be directed away from adequately functioning parts of the liver. We call this treatment approach ‘functional-avoidance radiation therapy’.”
Her hope is that this approach will improve survival and quality of life.
“Even small gains can make a big difference for patients and their families. Ultimately, I want to see liver cancer outcomes shift from limited options to real hope.”
Progress to a real-world clinical study
Dr Tadimalla and her team have developed an MRI protocol specifically for liver function measurements. With the method now validated, a PhD student is creating artificial-intelligence-based tools to do the mathematical modelling to extract liver function maps from the MRI data.
In a major step on the translational pathway, Dr Tadimalla’s research has progressed to a clinical trial at Westmead Hospital with the aim to expand in the future.
“I lead the trial alongside a team of specialists in radiation oncology, nuclear medicine, and hepatology at Westmead Hospital, as well as international collaborators. It is also supported by industry partners,” Dr Tadimalla said.
“We have presented early results at major conferences and are working with other hospitals to expand the study. It’s exciting to see this research moving closer to clinical translation.”
Dr Tadimalla credits her Cancer Institute NSW Fellowship as invaluable to her research.
“This Fellowship has provided the support needed to establish a clinical trial, build strong collaborations, and recruit a highly capable PhD student,” Dr Tadimalla said.
“It has laid the foundation for turning a research idea into a real-world clinical study with the potential to change practice.”
Support from the Cancer Institute NSW
Funding from the Cancer Institute NSW grant, worth more than $550,000, has built on Dr Tadimalla’s research and network capacity. It has also supported her career progression by helping her bridge academic expertise and clinical application.
“My expertise in MRI is now recognised within the radiation therapy community,” she said.
“I have been invited to join professional organisations and committees shaping the use of MRI in clinical trials. The annual Fellows Forum has also helped me connect with other researchers, share my work, and gain insights that have strengthened both the academic and clinical sides of my research.”
Dr Sirisha Tadimalla is a medical imaging physicist and researcher at the University of Sydney. See her bio. Find out more about Cancer Institute NSW’s fellowship recipients and their work.