
Journey
Aboriginal people across NSW are invited to share experiences of how cancer has impacted your community, your family, or yourself.
Community
By sharing your story, you will help shape the development and delivery of the NSW Aboriginal Cancer Strategy 2025-2027 and improve cancer services and experience for Aboriginal Peoples and Communities across NSW.
Sharing your story

Empowerment
Aboriginal Community Cancer Conversations
- Purpose: Screening and prevention
- People: Men’s and Women’s Business
Support
Aboriginal Client Conversations
- Purpose: Diagnosis, treatment, survivorship, palliative care, journey to dreaming
- People: Lived experience

Collaboration
Cancer Workforce Conversations
- Point of care
- Continuity of care
- Connection of care
Aboriginal Cancer Conversations | share your experiences online
NSW Digital Aboriginal Community Cancer Conversation Guide
Screening and Prevention
- Do you feel comfortable talking about screening and prevention?
- What would help make conversations about cancer screening more comfortable for you:
- Resources?
- Health Promotion days?
- Other
- How much do you know about cancer prevention?
- How much do you know about cancer screening?
- Are there any barriers to accessing cancer screening services:
- Geographical location
- Costs/financial
- Cultural safety
- Other
- What could help overcome the barriers?
- What would make cancer screening services more welcoming and accessible for you and your community?
- Do you feel like health professionals (doctors, nurses) provide culturally appropriate care during checkups?
Could you list 3 things that would make the space / check up room feel safer and more supportive? - For women’s business, are you comfortable attending services like BreastScreen or Women’s Health Services?
- Would having Aboriginal health workers involved in the screening process help you feel more at ease?
- Where do you usually get health information:
- Online
- GP clinics
- Aboriginal workforce
- Family
- Other
- Where do you usually get health information:
- Do you find the information on cancer screening easy to understand?
- How could cancer prevention and screening programs be better designed to meet the needs of your community?
- Have you had any cancer screenings in the past 12 months? If Yes,
- Bowel screening
- Cervical screening
- Breast screening
- Do you have any suggestions to support community in accessing screening services within your community?
Diagnosis, Treatment, Survivorship, and Palliative Care
Impact of cancer: I have cancer, I have supported someone with cancer, I have had cancer, I prefer not to say,
- What challenges have you or other mob face by the burden of cancer.
- Which of these burdens is the most important to fix. Which one would have the biggest impact?
- What is important to you in your Cancer Treatment. (list 5 things that matter to you during your cancer journey)
- Where were the gaps in your experience with cancer?
- Prompt: What help did you need? (food, washing of clothes, transport, financial aid, Spiritual Social Emotional Wellbeing, Navigating Hospital Health Service, Referral to Support Teams (Social Work, Psych), Linking into Aboriginal Workforce Liaisons, Other)
- What area of the cancer experience would you like to see improved?
- What would make it easier for you and your family to communicate and navigate your needs and questions to healthcare providers?
- E.g. Aboriginal Hospital Liaison Officers / Workforce, Appropriate Resources to understand treatment, Follow-Up contact information.
- How did you go translating western medical terminology? Were you able to translate or needed assistance? If you needed support, who provided it?
- How important is it for you, family and kin to have Aboriginal and Torres Strait Islander workforce involved in your treatment journey?
- Would having culturally specific resources help you feel more supported during your cancer treatment?
- How accessible are the existing cancer care health services for you, family and kin?
- Are there specific challenges using the services?
- What could we do to enhance the accessibility of services?
- What ongoing support is important after completing your cancer treatment?
- How can health care providers or the cancer care workforce support your journey back to community?
- How important is community, family and kin’s involvement in the recovery process?
- Would connecting with Aboriginal and Torres Strait Islander survivors in your area (or online) be helpful?
- Is there any wisdom you’d like to share in the cancer survivorship journey?
Digital form now open: Aboriginal Cancer Conversations Survey
Close date of form: Friday 28th February 2025
A number of in person and virtual sessions were held across NSW, in collaboration with local Aboriginal Community Controlled Organisations.
These conversations:
- Created space to identify the challenges and solutions being experienced by Aboriginal people accessing cancer services and support.
- Will help to design support for clients, kin and carer’s who have been affected by cancer.
- Provided an opportunity to improve cultural responsiveness for cancer services and support.
What questions were asked?
The Cancer Institute NSW and Aboriginal Health and Medical Research Council of NSW is committed to the development of a NSW Aboriginal Cancer Strategy 2025 – 2027.
It is anticipated that this Strategy will align to the NSW Aboriginal Health Plan 2024 – 2034, NSW Cancer Plan 2022 – 2027 and NACCHO Aboriginal and Torres Strait Islander Cancer Plan.
To ensure we heard the voices of cancer clients, community members, cancer and support services we carried out Aboriginal Cancer Conversations through various mediums. Below is a guide to these conversations that were held.
Regional Webinar Aboriginal Community Cancer Conversation Guide
- Do you feel comfortable talking about screening and prevention?
- What would help make conversations about cancer screening more comfortable for you?
- What do you know about cancer screening?
- What have you heard about getting checked?
- How does it make you feel?
- Are there any barriers to accessing cancer screening services: (Eg: geographical location? costs/financial? cultural safety? Anything else?
- What could help overcome them?
- What would make cancer screening services more welcoming and accessible for you and your community?
- Do you feel like health professionals (doctors, nurses) provide culturally appropriate care during check-ups and screening?
- Could you tell us three things what would make the space/check up room) feel safer and more supportive?
- For women’s business, are you comfortable attending services like BreastScreen or Women’s Health Services?
How could these services be more culturally safe? - Would having Aboriginal health workers involved in the screening process help you feel more at ease?
- Where do you usually get health information:
- Online
- GP clinics
- Aboriginal workforce
- Family
- Other
- Do you find the information and resources on cancer screening easy to understand?
- What could improve this?
- How would you like to share with family and kin?
- How can we encourage younger or older community members to participate in cancer prevention and screening?
- How could cancer prevention and screening programs be better designed to meet the needs of your community?
- Do you have experience of cancer screening in the past 12 months? If comfortable to share, can you tell us more?
- Bowel screening
- Cervical screening
- Breast screening
- What challenges have you or other mob face by the burden of cancer.
- Which of these burdens is the most important to fix.
- Which one would have the biggest impact?
- What is important to you in your Cancer treatment.
- Where were the gaps in your experience with cancer?
- What help did you need? (food, washing of clothes, transport, financial aid, spiritual, emotional, and overall wellbeing)
- What area of the cancer experience would you like to see improved?
- What would make it easier for you and your family to communicate and navigate your needs and questions to healthcare providers?
- Understanding your diagnosis?
- How did you go translating western medical terminology?
- Were you able to translate or needed assistance?
- If you needed support, who provided it?
- How important is it for you, family and kin to have Aboriginal and Torres Strait Islander workforce involved in your treatment journey?
- Would having culturally specific resources (informational materials, support groups) help you feel more supported?
- How accessible are the existing cancer care health services for you, family and kin?
- Are there specific challenges using the services?
- If yes, what could we do to enhance the accessibility of services?
- What ongoing support is important after completing your cancer treatment?
- How can health care providers or the cancer care workforce support your journey back to community?
- How important is community, family and kin’s involvement in the recovery process?
- Would connecting with Aboriginal and Torres Strait Islander survivors in your area (or online) be helpful?
- Is there any wisdom you’d like to share in the cancer survivorship journey?
- If yes, would you like to be involved in a mob mentor peer support group?
- From your perspective, what are the key challenges that mob face when accessing cancer care.
- Based on your experience, what tasks should be prioritised in the daily role of a cancer coordinator role?
- What do you consider essential principles to include in a culturally responsive cancer care model for mob?
- Are there any specific resources, training or skills that you feel are necessary for someone in the cancer coordinator role?
- How do you currently capture or track the patient journey?
- What additional elements would you like to see included in the figure to better reflect cultural and practical needs?
- What do you think are the biggest gaps in the delivery of cancer care for mob?
- How could these gaps be addressed within the model we are developing?
- When referring patients to services?
- Who are you referring to? (AMS, Cancer Council, McGrath Foundation)
- How do you place referral? (electronic, paper, phone call, email)
- What are the relationships between health services in your area?
- How do you feel we can best support Cancer Coordinators in their / your roles?
What support was available?
Support was available during the sessions to ensure participants felt comfortable and safe. A trained Aboriginal facilitator guided the discussion, and confidentiality was respected.
When were the sessions and who participated?
Aboriginal Cancer Conversations | webinars for regional communities

LHDs: Hunter New England LHD, Northern NSW LHD and Mid North Coast LHD
Date: Tuesday 21st January 2025
Time: 9:30am – 10:30am

LHDs: Western NSW LHD and Far West LHD
Date: Tuesday 21st January 2025
Time: 12:00pm – 1:00pm
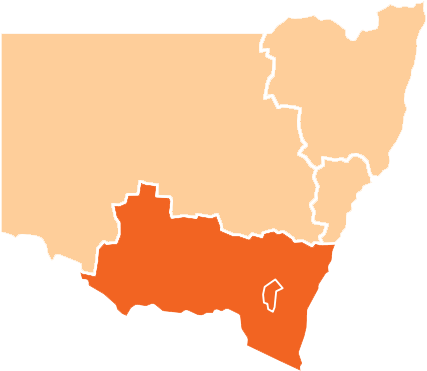
LHDs: Murrumbidgee LHD and Southern NSW LHD
Date: Wednesday 22nd January 2025
Time: 9:30am – 10:30am
Metropolitan Region

LHDs: Nepean Blue Mountains LHD, Central Coast LHD, Western Sydney LHD, Northern Sydney LHD, Sydney LHD, South Eastern Sydney LHD, South Western Sydney LHD and Illawarra Shoalhaven LHD
Date: Wednesday 22nd January 2025
Time: 12:00pm – 1:00pm
Find out more about the impact of cancer in your communities.
What will happen after the sessions?
After the sessions, we will share a summary of how your feedback has contributed to shaping the Aboriginal Cancer Strategy 2025-2027.
RSVP
If you would like to RSVP or ask a question, please contact us via cinsw-shareyourstory@health.nsw.gov.au.

Yabun Festival takes place annually on January 26th and is the largest community led one-day festival of Aboriginal and Torres Strait Islander cultures.
The report provides an overview of cancer in Aboriginal people and covers cancer prevention, cancer screening, diagnosis and treatment the common cancers diagnosed in Aboriginal people in NSW.

