Screening updates
Jump to:
2026 program news and updates
2025 program news and updates
- November 2025
- New campaign aims to increase participation in lung cancer screening/a>
- October 2025
- Cervical Screening: Empowering Choice Through Self Collection
- New National Bowel Cancer Screening Program Healthcare Provider Learning Hub
-
September 2025
- NSW Cervical Screening Program newly launched resource
- Help us improve colonoscopy access in NSW by sharing your story
- August 2025
- New cervical screening during pregnancy resources available in more than 20 languages
- National Lung Cancer Screening Program now available for eligible Australians
- July 2025
- The 2025 winter season is here
- Revised National Cervical Screening Program Clinical Guidelines and core changes
- Latest updates on the National Lung Cancer Screening Program
- June 2025
- Latest updates on the National Lung Cancer Screening Program
- May 2025
- BreastScreen NSW to begin informing women of their breast density
- Latest updates on the National Lung Cancer Screening Program
- April 2025
- Join the ReadytoScreen trial to support lung cancer screening
- February 2025
- January 2025
- New screening program to reduce lung cancer risk
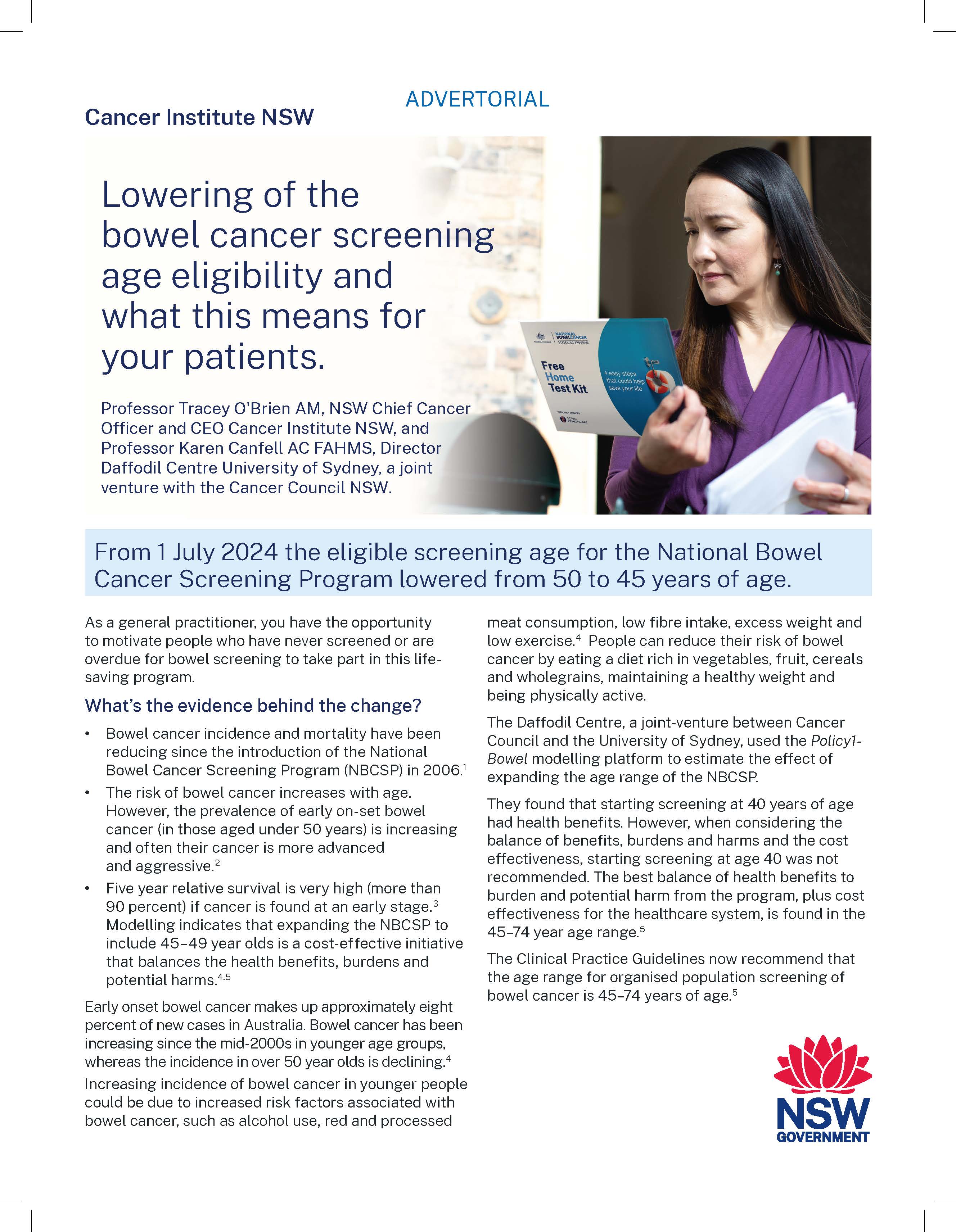
- Lowering of the bowel cancer screening age eligibility and what this means for your patients
2024 program news and updates
-
December 2024
-
November 2024
- GPs needed to help codesign a new referral tool for colonoscopy! -
October 2024
- ‘Own It’ & ‘Screen Me’ National Cervical Screening Campaigns
- October is breast cancer awareness month -
September 2024
- National Lung Cancer Screening Program set to Launch in July 2025
- National Bowel Cancer Screening Community Roadshow -
August 2024
- Have your say: education needs for the upcoming National Lung Cancer Screening Program
- Bowel Cancer Screening Program: Eligibility age lowering and alternative access to kits for healthcare providers
- GPs needed for feedback around improving colonoscopy referrals
- NEW GP cancer screening kits with translated materials -
July 2024
- New Lung Cancer Screening Program website and resources now live!
- HPV Self-Collection: Are YOU ready to support the choice? -
June 2024
- What is your local bowel cancer screening participation rates? Share our Bowel Screening QI module for Bowel Cancer Awareness month. -
May 2024
- NEW BreastScreen NSW website with easy breast screening booking and health professional resources
- Catch up on the latest RACGP and Cancer Institute NSW Webinar! -
February 2024
- Swab the Facts: Cervical Screening Self-Collection
- BreastScreen Australia – Public consultation NOW OPEN
- Pregnancy and cervical screening: Everything GP Shared Care Program providers need to know
February 2026 news and updates
Breast cancer doesn’t wait, so don’t wait to breast screen
More than 579,00 women in NSW are overdue for their recommended two-yearly breast screen, meaning thousands may be living with undiagnosed breast cancer.
In response, BreastScreen NSW has re‑launched its successful Breast Cancer Doesn’t Wait behaviour change campaign to motivate women in NSW to book a breast screen when due.
The campaign warns that “breast cancer doesn’t wait” for life to slow down and encourages women to prioritise a breast screen despite busy schedules.
The 2025 Breast Cancer Doesn’t Wait campaign achieved an estimated 22 per cent increase in bookings – an additional 12,000 bookings among eligible women. This year’s campaign builds on those efforts by focusing more strongly on communities with lower screening rates, including Mandarin and Cantonese speaking women, and Aboriginal women aged 40-74.
Targeted initiatives will focus on local government areas such as Blacktown, Canterbury‑Bankstown, Cessnock, Coffs Harbour, Cumberland, Dubbo Regional, Fairfield, Liverpool, Maitland, Nambucca Valley, Port Macquarie, Richmond Valley and Shellharbour.
A tailored campaign, Stay Strong, Black & Deadly, for Aboriginal and Torres Strait Islander women, features a powerful testimonial from Jacqui Khan, a proud Gomeroi woman, who shares how a routine breast screen detected her breast cancer early.
Aboriginal and Torres Strait Islander women continue to experience poorer breast cancer outcomes including lower survival rates, more advanced tumours at diagnosis, and lower participation in breast screening programs. BreastScreen NSW aims to close this gap and ensure more women have access to early detection and life-saving screening.


November 2025 news and updates
New campaign aims to increase participation in lung cancer screening
The National Lung cancer Screening Prpgram (NLCSP) offers eligible participants a free low-dose computed tomography (CT) scan every 2 years to detect lung cancer early, before symptoms appear.
Lung cancer is the leading cause of cancer-related death. However, when detected early through screening, more than 65% of cases can be successfully treated.
As a healthcare provider, you play a critical role in the delivery of the program. The new campaign will help drive important conversations and ensure more Australians can benefit from early detection.
With this campaign now launched, it is expected that more patients will be presenting to primary care clinics for information and referral.
To access more information about the screening program, including how you can support your clients, visit the NLCSP website.
October 2025 news and updates
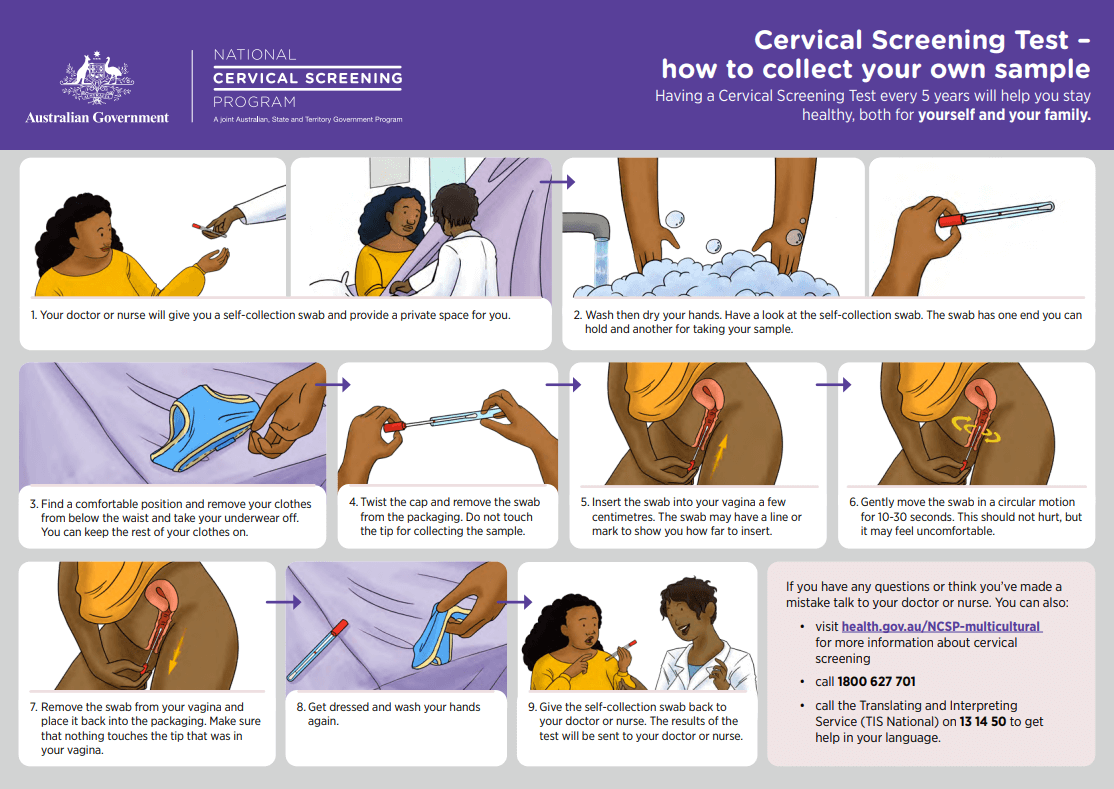
Cervical Screening: Empowering Choice Through Self Collection
More than 70% of cervical cancers occur in people who have never been screened or are not up to date with their cervical screening. Increasing participation is critical and self-collection offers a powerful tool to help achieve this.
Self-collection provides patients with greater control and choice, removing a significant barrier to screening. It may be especially acceptable to groups who are less likely to screen, including:
- Aboriginal and/or Torres Strait Islander peoples
- Culturally and linguistically diverse communities
- LGBTIQ+ individuals
- People with disabilities
- Survivors of sexual violence
- Post-menopausal individuals
- Those with previous negative screening experiences
A recent study by the University of Sydney found that fewer than half of patients were offered a choice at their most recent screening. Many participants lacked awareness of their options and felt unprepared to make informed decisions. While not all preferred self-collection, most valued having a choice and recognised its benefits for others. The attitudes and communication of healthcare providers strongly influenced their decision-making.
Evidence shows that self-collection can significantly improve participation. In one pilot, 85.7% of never- or under-screened individuals who declined a speculum exam agreed to self-collect when the test was offered in a sensitive and culturally appropriate manner, with appropriate follow-up advice.
Self-collection is available any time an HPV test is needed, including for follow-up testing after an intermediate risk result. If HPV is detected on a self-collected vaginal sample, follow-up may include :
- A clinician-collected cervical sample for liquid-based cytology, or
- Referral to a specialist, depending on the HPV type detected
Healthcare providers must have clear pathways to ensure timely follow-up for screen-detected abnormalities. While clinician observation of sample collection is not required, it can be offered if preferred by the patient .
Self-collection should be offered in clinic settings wherever possible but can also be provided in other settings at the discretion of the supervising healthcare provider with the goal of maximising participation.
For more information, please refer to Cervical Cancer Screening Guidelines | Cancer Council.
References:
1. https://www.cancer.nsw.gov.au/prevention-and-screening/screening-and-early-detection/cervical-screening/cervical-screening-for-health-professionals/self-collection-key-messages
2. https://pubmed.ncbi.nlm.nih.gov/40829929/
New National Bowel Cancer Screening Program Healthcare Provider Learning Hub

GPEx, in partnership with the Australian Government, has launched a national education initiative to support healthcare providers in encouraging participation in the National Bowel Cancer Screening Program.
Healthcare providers—including GPs, nurses, practice staff, tertiary specialists, and allied health professionals, now have access to:
- Free, CPD accredited training events
- Downloadable resources to support bowel screening conversations
- An online Learning Hub with everything you need to know about the National Bowel Cancer Screening Program and the cancer care continuum
Empower your patients by starting the conversation — early detection of bowel cancer saves lives.
Learn more, gain CPD hours, and enrol in the free bowel cancer screening learning options at www.gpex.com.au/nbcsp-education.
September 2025 news and updates
NSW Cervical Screening Program newly launched resource

Cervical cancer is one of the most preventable cancers, and Australia is on track to become the first country to equitably eliminate it. Achieving this goal depends on maintaining and improving screening and early detection rates, ensuring that all eligible individuals with a cervix are offered timely cervical screening and appropriate follow-up care.
Primary care providers are central to this effort. To support your conversations with patients, new resource is now available on colposcopy. This tool aligns with the updated National Cervical Screening Program (NCSP) Clinical Guidelines, released in April 2025.
Colposcopy – What You Need to Know: Colposcopy plays a key role in identifying high-risk HPV and early cervical changes that may require further monitoring or treatment. The new colposcopy resource is designed to support patients through easy-to-understand language during the referral process and serve as a reference after your consultation.
Available formats: Web resource, Printable factsheet in plain English and Audio file and is available in ten community languages.
It provides patients with clear, plain-English explanations of what to expect during and after a colposcopy, reinforces your clinical advice and helps reduce anxiety or confusion and supports patients with low literacy through audio versions.
Help us improve colonoscopy access in NSW by sharing your story
With services established in almost all regions of NSW, Direct Access Colonoscopy (DAC) services are key to reducing wait times, costs and anxiety for patients following a positive bowel screening test.
Primary care practitioner involvement in colorectal cancer screening and colonoscopy referrals are crucial to improving colorectal cancer outcomes. The chosen referral pathway will affect how a patient is assessed prior to the procedure (in-person or over the phone), their out-of-pocket costs, and the time they will need to wait to have their procedure.
A 2024 survey of NSW GPs found that awareness of DAC remains low. For example, half of participating GPs practicing in areas with a public DAC service had not heard about this option, and most were unsure about the eligibility criteria for referral.
As part of our ongoing efforts to raise awareness, we’re looking to speak to GPs and patients who would be willing to share their stories of how access to a DAC service benefited them or their patients. Quotes from interviews or surveys may be used across stories and advertising in primary care targeted publications and social media to help spread the word.
August 2025 news and updates
National Lung Cancer Screening Program now available for eligible Australians
The resources provide clear, engaging information to help pregnant women, and the maternity workforce, learn about cervical screening and encourage those who are due to have it done as part of routine pregnancy care.
English resources:
- Information about cervical screening during pregnancy (webpage), including option to listen to audio recording
- Factsheet for pregnant women (PDF)
- Poster – A3 printed posters for clinics/waiting rooms with QR code
- Digital Poster (PowerPoint) for digital screens in clinics/waiting rooms
- Mouse Pad for clinic rooms, to encourage conversations with patients, with a QR code to information for health professionals
Translated resources:
- In-language resources are easily accessible on the Cancer Institute NSW website, including in-language webpages, PDF factsheets and audio recordings.
- More than 20 languages are available, including Arabic, Bengali, Burmese, Cantonese, Dari, English, Farsi, Gujarati, Indonesian, Japanese, Korean, Mandarin, Nepali, Portuguese, Punjabi, Spanish, Tagalog, Thai, Turkish, Urdu, and Vietnamese.
We encourage you to view the resources on our website and share these with your stakeholders or email us to order printed copies of the poster.
New cervical screening during pregnancy resources available in more than 20 languages
Helpful resources
- Commonwealth website has been updated to support the launch, featuring new materials and content. has been updated to support the launch, featuring new materials and content.
- A suite of resources is available on the Commonwealth website. These are being translated into 21 languages - Arabic, Assyrian, Simplified Chinese, Traditional Chinese, Dari, Greek, Hazaragi, Hindi, Indonesian, Italian, Khmer, Korean, Macedonian, Nepali, Persian (Farsi), Punjabi, Serbian, Spanish, Thai, Turkish, Vietnamese.
- NACCHO website - resources to support eligible Aboriginal and Torres Strait Islander people and their families. Includes the Making Decisions Together model resources to participate in shared decision-making about lung cancer screening with their healthcare professionals.
Helpful resources
- Commonwealth website has been updated to support the launch, featuring new materials and content. has been updated to support the launch, featuring new materials and content.
- A suite of resources is available on the Commonwealth website. These are being translated into 21 languages - Arabic, Assyrian, Simplified Chinese, Traditional Chinese, Dari, Greek, Hazaragi, Hindi, Indonesian, Italian, Khmer, Korean, Macedonian, Nepali, Persian (Farsi), Punjabi, Serbian, Spanish, Thai, Turkish, Vietnamese.
- NACCHO website - resources to support eligible Aboriginal and Torres Strait Islander people and their families. Includes the Making Decisions Together model resources to participate in shared decision-making about lung cancer screening with their healthcare professionals.
Program guidelines
- Updated to reflect nurse practitioners’ role in the program, links to new resources such as the NCSR forms and rules, and to reflect the final MBS item names.
NLCSP low-dose CT request form
- The program-specific request form is designed to capture all necessary clinical details to support a radiologists’ decision-making in line with the Nodule Management Protocol.
- Available in Communicare, Best Practice, Medical Director, and MMEX clinical information software. PDF and word document versions are also available.
Healthcare provider strategy
- Education packs are being prepared, with the first batch expected for delivery early July.
- The Digital Stakeholder Toolkit is available online.
Working with PHNs
- The first PHN working group meeting was held in June to discuss what PHNs need and how the Commonwealth can help them in supporting primary care providers.
- Regular meetings with the PHN working group will be held moving forward.
NCSR updated to include NLCSP:
- The NCSR website has been updated with helpful links, guides and documents relevant to the NLCSP.
- Finalising five primary program forms within the NCSR, which can be accessed through integrated clinical software, the NCSR Healthcare Provider Portal and online.
- User guides, communications products and other assets will be updated to include NLCSP to support consumers and healthcare providers use the NCSR for the NLCSP.
- Telstra Health has worked closely with Radiology Information Systems vendors on NCSR integration. A number of major providers will be integrated from 1 July, with the majority within the first 6 months.
TSANZ education strategy
- TSANZ has been engaged to deliver an education strategy to demonstrate how to report on participant outcomes using the NLCSP Diagnosis Form in the NCSR Healthcare Provider Portal.
TSANZ are hosting a webinar on the use of the NLCSP Diagnosis form on 4 August 2025. Register online here.
July 2025 news and updates
The 2025 winter season is here
The 2025 winter season is here. Influenza (flu) activity has increased over the last 4 weeks. The influenza vaccine is recommended now to protect people at higher risk of severe illness, including cancer patients. Cancer is an immunocompromising condition and the influenza vaccine is free for these Medicare-eligible patients.
International trends show the possibility of high influenza activity in 2025 and increased influenza B which can have a greater impact on children.
The NSW respiratory surveillance report is a great way to keep track of current respiratory virus activity levels in the community, including the latest rates of respiratory illness specific to your local area.
Program guidelines
- Updated to reflect nurse practitioners’ role in the program, links to new resources such as the NCSR forms and rules, and to reflect the final MBS item names.
NLCSP low-dose CT request form
- The program-specific request form is designed to capture all necessary clinical details to support a radiologists’ decision-making in line with the Nodule Management Protocol.
- Available in Communicare, Best Practice, Medical Director, and MMEX clinical information software. PDF and word document versions are also available.
Healthcare provider strategy
- Education packs are being prepared, with the first batch expected for delivery early July.
- The Digital Stakeholder Toolkit is available online.
Working with PHNs
- The first PHN working group meeting was held in June to discuss what PHNs need and how the Commonwealth can help them in supporting primary care providers.
- Regular meetings with the PHN working group will be held moving forward.
NCSR updated to include NLCSP:
- The NCSR website has been updated with helpful links, guides and documents relevant to the NLCSP.
- Finalising five primary program forms within the NCSR, which can be accessed through integrated clinical software, the NCSR Healthcare Provider Portal and online.
- User guides, communications products and other assets will be updated to include NLCSP to support consumers and healthcare providers use the NCSR for the NLCSP.
- Telstra Health has worked closely with Radiology Information Systems vendors on NCSR integration. A number of major providers will be integrated from 1 July, with the majority within the first 6 months.
TSANZ education strategy
- TSANZ has been engaged to deliver an education strategy to demonstrate how to report on participant outcomes using the NLCSP Diagnosis Form in the NCSR Healthcare Provider Portal.
TSANZ are hosting a webinar on the use of the NLCSP Diagnosis form on 4 August 2025. Register online here.
Revised National Cervical Screening Program Clinical Guidelines and core changes
The National Cervical Screening Program (NCSP) guidelines have recently been reviewed and updated by Cancer Council Australia, under contract with the Department of Health and Aged Care. These updates aim to ensure alignment with the latest evidence and best clinical practice in the management of screen-detected abnormalities, screening in specific populations, and investigation of abnormal vaginal bleeding.
To maintain the effectiveness and safety of the NCSP, the guidelines have been revised to reflect current evidence and clinical consensus. These updates are designed to support healthcare providers in delivering optimal care and to ensure consistency in the management of cervical screening outcomes across Australia.
While a number of revisions have been made, three core changes are particularly important for clinical practice:
- Test of Cure (ToC) Management: Updated protocols for managing patients’ post-treatment to ensure appropriate follow-up and reduce unnecessary interventions.
- Surveillance After Treatment for Adenocarcinoma in Situ (AIS): Revised recommendations for ongoing surveillance of patients treated for glandular abnormalities.
- Post-Total Hysterectomy ToC and AIS Testing: Clarified guidance on when and how to conduct follow-up testing in patients who have undergone total hysterectomy.
To support you in applying the updated guidelines in your practice, the following resources are available:
Full Revised Guidelines: https://www.cancer.org.au/clinical-guidelines/cervical-cancer/cervical-cancer-screening
2-Page Quick Reference Guide for Providers: https://www.cancer.org.au/assets/pdf/cervical-screening-quick-reference-guide
Summary Guide for Healthcare Providers (see pages 11, 16, and 17): https://www.cancer.org.au/assets/pdf/ncsp-summary-guide-for-health-care-providers
Additionally, communication has been sent, by the National Cervical Screening Program, directly to screening participants to inform them of these changes, encouraging them to discuss any questions with their primary care provider.
Now live: Refer4Scope. Supporting GPs to make guideline-appropriate colonoscopy referrals in a few clicks.

We are excited to announce the launch of Refer4Scope – a new online decision tool, designed to support primary care practitioners make guideline-appropriate colonoscopy referrals in just a few clicks.
Primary care professional’s referrals for colonoscopy are crucial for enhancing the efficiency and effectiveness of colorectal cancer detection and treatment. The referral pathway to colonoscopy can affects how a patient is assessed prior to the procedure (in-person or over the phone), their out-of-pocket costs, and the time they will need to wait to have their procedure.
Designed to save time mid-consult, GPs can follow the simple prompts to enter their patient’s age, screening test outcomes, bowel symptoms and/or family history of colorectal cancer to receive the recommended next step as well as additional resources.
Refer4Scope was developed by the Daffodil Centre with support from the Institute. It was created by leading experts and co-designed with clinicians; and draws from the 2023 update to the Clinical practice guidelines for the prevention, early detection and management of colorectal cancer.
Access the tool here: www.cancer.nsw.gov.au/refer4scope
The tool has also been added to several NSW HealthPathways sites to further support GPs in accessing it at the point of care.
July updates on the National Lung Cancer Screening Program

Preparing for the NLCSP
- A helpful checklist is available to provide information on preparing your practice so it is ready for the Program launch in July 2025.
Education and resources
- The Commonwealth has published new resources for the health sector on their website. NLCSP guidelines and additional resources relating to the program can also be found here.
- Lung Foundation Australia and Daffodil Centre have launched educational resources for the NLCSP.
- Six self-paced modules guide health professionals through the step-by-step screening process, gaining practical insights into how early detection can significantly enhance patient outcomes.
- Learn more and enrol in the modules here.
- Webinars to watch on demand:
- I-MED Radiology Network provided online webinar, ‘From Early Detection to Lifesaving Action - Navigating the National Lung Cancer Screening Program’ on Tuesday 13 May 2025. The webinar is available to watch on demand here.
- National Lung Cancer Screening Program Health Workforce Education Webinar is available on demand by registering here.
- RACGP ‘The National Lung Cancer Screening Program: What GPs need to know’ webinar is available on demand here.
Heart of Australia (HoA) mobile CT services for NSW:
- Commonwealth and HoA, alongside representatives from NACCHO, AH&MRC, Cancer Institute NSW and Rural Health, met in late May to plan for introduction of a mobile CT service.
- Consultation and route planning for NSW will continue, with the aim to finalise this by September 2025.
HealthPathway:
- The NLCSP HealthPathway is now live and has been disseminated in NSW and nationally. Individual PHN localisation can occur before local release (as required).
Imaging:
- Private imaging providers across NSW have indicated their willingness to participate in NLCSP.
- Several private providers across NSW are promoting the NLCSP on their websites and encouraging consumers to consult with their GP to obtain a referral for LDCT.
June 2025 news and updates
Latest updates on the National Lung Cancer Screening Program

Lung Cancer HealthPathway
- Development of the HealthPathway is being finalised following the publication of the National guidelines.
Preparing for the NLCSP
- A helpful checklist is available to provide information on preparing your practice so it is ready for the Program launch in July 2025.
Educational resources
- The Department has published the NLCSP guidelines and resources relating to the program on their website.
- These resources will support the healthcare sector to facilitate a participant’s entire screening journey, including guidelines and information about preparing to offer the program, determining eligibility, starting conversations, providing support for participants, and answers to frequently asked questions.
- Lung Foundation Australia and Daffodil Centre will launch educational resources for the NLCSP.
- Training and supporting resources will guide health professionals through the step-by-step screening process, gaining practical insights into how early detection can significantly enhance patient outcomes.
- Training consists of six self-paced modules which will take around 3.5 hours total to complete. Participants can earn 3.5 Continuing Professional Development points.
- Learn more and express your interest here.
- Webinars available for registration:
- National Lung Cancer Screening Program Health Workforce Education Webinar is available on demand by registering here.
- The RACGP ‘National Lung Cancer Screening Program: What GPs need to know’ webinar will be held on 3rd June 7:30pm. Register here.
Travel scheme to support screening
- It is confirmed that this will be managed by the Commonwealth and is for screening only.
- Further information to be provided as to when the scheme will become available.
Heart of Australia mobile CT services for NSW
- The mobile CT screening service commence in 2027.
- CINSW continues to meet with the Commonwealth, Heart of Australia and other jurisdictions to finalise route planning.
Are your patients screening for bowel cancer?

Bowel cancer is state’s second deadliest cancer yet only two out of every five people eligible for the test in NSW are currently participating.
The National Bowel Cancer Screening Program’s lifesaving test is quick and easy to do and can be completed at home in minutes. Those who have done it before are almost three times more likely than first-time invitees to do it when it arrives in the mail.
The screening test – available for those aged between 45-74 years – is the easiest way to detect the early signs of bowel cancer, which if caught early can be successfully treated in more than 90 per cent of cases.
GPs can refer patients to the National Bowel Screening Register to request a kit themselves. For those who need support with this, there is an option for GPs to complete the form on their patients’ behalf.
People can reduce their risk of bowel cancer by eating a diet rich in vegetables, fruit, cereals and wholegrains, maintaining a healthy and weight and being physically active; and by doing the screening test every two years from 45.
May 2025 news and updates
BreastScreen NSW to begin informing women of their breast density
By the end of April, BreastScreen NSW will be advising women of their breast density to help them better understand their breast cancer risk and make more informed decisions about their breast health.
Breast density is the ratio of fibroglandular tissue to fatty tissue in the breast. It’s estimated around 40 per cent of women who have screened with BreastScreen NSW have dense breast tissue.
Breast density reporting will be phased over the coming months using new technology recently implemented by BreastScreen NSW. This will take place as part of a woman’s routine breast screen and won’t change the screening experience in any way.
Clients will be encouraged to speak with their GP if they have concerns about their breast density, in the context of their other risk factors, personal circumstances and preferences.
Understanding breast density
Extremely dense breast tissue can in some cases, reduce the visibility of cancers on a mammogram. Breast density cannot be felt and is not linked to breast size or shape. For most women, density changes over time and reduces with age.
While breast density is a known risk factor for breast cancer, age is the biggest risk factor, with more than 75 per cent of breast cancers occurring in women over 50. Family history, genetic, reproductive and modifiable risk factors like diet and alcohol consumption can also increase a person’s risk of the disease.
BreastScreen NSW clients and their nominated GP will be provided with a BI-RADS classification in screening results letters and supported with updated information on the BreastScreen NSW website.
Reporting for all clients who screen will be phased in over coming months with reporting for those attending assessment clinics to follow later in 2025.
Everyone is unique
Everyone’s circumstances are unique, so we recommend women who are concerned or have questions, have a discussion with their GP about their individual risk factors for breast cancer.
Regardless of their breast density, women are recommended to have their regular mammograms.
Refer4Scope - Learn about this new colonoscopy referral decision tool in an upcoming educational webinar

To support GPs and patients, the Daffodil Centre, proudly supported by the Cancer Institute NSW, have developed an online decision tool to encourage guideline appropriate assessment, triage and referral for colonoscopy services by primary care practitioners in NSW.
Training to use the tool will be provided to GPs as part of a webinar, presented by the Daffodil Centre in partnership with the Cancer Institute NSW.
Afterwards, participants will be equipped with up-to-date knowledge and access to the practical online tool, called Refer4Scope, enabling them to provide guideline appropriate recommendations to manage colorectal cancer risk and appropriately triage and refer for colonoscopy services in NSW.
This webinar will address the following key learning areas:
Date: Thursday 12 June 2025
Time: 7:00 – 8:30 pm
Registration: Free, register here
This webinar has been accredited by the RACGP for 1.5 Educational Activity hours.
This webinar has been developed by the Daffodil Centre and funded by the NSW Government through the Cancer Institute NSW.
Latest updates on the National Lung Cancer Screening Program

Lung Cancer HealthPathway
- Development of the HealthPathway continues and will be completed when final program guidelines and resources are released.
Educational resources
-
- Lung Foundation Australia and Daffodil Centre will launch educational resources for the NLCSP.
- Training and supporting resources will guide health professionals through the step-by-step screening process, gaining practical insights into how early detection can significantly enhance patient outcomes.
- Training consists of six self-paced modules which will take around 3.5 hours total to complete. Participants can earn 3.5 Continuing Professional Development points.
- Learn more and express your interest here.
Heart of Australia mobile CT services for NSW
NLCSP Nurse Practitioner role
Seeking participants for the ‘Ready to Screen’ Trial
April 2025 news and updates

Join the ReadytoScreen trial to support lung cancer screening
Why lung cancer screening?
The National Lung Cancer Screening Program will begin on 1st July 2025, and eligible participants will need a referral from their GP to be screened. Early detection through screening is proven to significantly improve outcomes for patients at high risk of lung cancer.
Is your practice prepared?
The ReadytoScreen trial aims to identify the most effective strategies for engaging eligible patients to take up lung cancer screening. The trials aims to understand how communication and information from a patient’s general practice can increase participation rates, and how practices can be better supported to deliver the National Lung Cancer Screening Program. The barriers and enablers to implementing the program will also be explored.
What’s involved in participating?
By joining the ReadytoScreen trial, your practice will:
These activities will ensure that your practice is prepared for roll-out of the National Lung Cancer Screening Program from July 1st 2025.
Eligibility criteria:
To participate, your practice must:
February 2025 news and updates
BreastScreen NSW’s ‘Breast cancer doesn’t wait’ campaign
The campaign runs from 16 February to 12 April 2025 across a range of mass media channels including television, radio (voiced by Australian entertainers, Kat Stewart and Amanda Keller), outdoor, broadcast video on demand, print, online video, digital display, paid search, and social media.
The campaign primarily targets women in NSW aged 50–64, including Cantonese and Mandarin-speaking women in NSW aged 50-74, as well as Aboriginal and Torres Strait Islander women in NSW aged 40-74.
For more information about the campaign visit www.breastscreen.nsw.gov.au/campaigns/breast-cancer-doesnt-wait-campaign
The Cancer Institute NSW is encouraging GPs and primary care professionals across the state to support the campaign by encouraging their clients to book a free breast screen.
Revised National Cervical Screening Program Guidelines
As 5 years have passed since Australia's National Cervical Screening Program (NCSP) transition to a screening strategy based on human papillomavirus (HPV) testing, the National Cervical Screening Program Guidelines have undergone a review and update. The scope of the review was informed by the NCSP clinical expert panel, and the update has involved evidence reviews, analysis of data from the first 5 years of HPV-based screening, and consultation with experts.
The revised NCSP Guidelines are now live and are available at: Cervical Cancer Screening Guidelines | Cancer Council
Resources to support these changes are incorporated within the guideline for quick access. These are:
The revised NCSP Guidelines are supported with the following healthcare provider training:
The National Cervical Screening Program (NCSP) has advised that changes will not go live in the National Cancer Screening Register (NCSR) until April. Discretion and best clinical judgement are to be used regarding the use and ‘compliance’ with the Guidelines during this time.
For any questions or concerns, please contact NCSP via NCSPcommittees@health.gov.au
January 2025 news and updates
New screening program to reduce lung cancer risk
The Australian Government is set to launch a National Lung Cancer Screening Program in July 2025. The new screening program presents a significant opportunity to increase early diagnosis, enhance treatment options and improve survival for people with lung cancer in NSW.
To understand if your patients will be eligible read National Lung Cancer Screening Program.
Lowering of the bowel cancer screening age eligibility and what this means for your patients
On 1 July 2024 the eligible screening age for the National Bowel Cancer Screening Program was lowered from 50 to 45 years.
The Cancer Institute has created a summary of the evidence behind the change, what it means for your patients, how you can better support Aboriginal and Torres Strait Islander patients, along with resources links for both you and your patients. As a general practitioner, you have the opportunity to motivate people who have never screened or are overdue for bowel screening to take part in this life-saving program.
To find out more: Bowel Cancer Screening and what this means for your patients
December 2024 news and updates
LGBTQ+ Bowel Screening Research

LGBTQ+ people have diverse needs and face unique barriers to accessing health services, including fear of and experiences of discrimination which may cause them to avoid or delay seeking healthcare. This includes barriers to accessing colonoscopy services following a positive bowel cancer screening test.
ACON has engaged Nous Group (Nous) to conduct research to improve access to and uptake of colonoscopy services for LGBTQ+ people who have received a positive bowel cancer screening test. We also aim to identify opportunities to improve the competency and knowledge of healthcare professionals to ensure delivery of high-quality, appropriate and inclusive colonoscopy services to LGBTQ+ people.
If you are involved in referring, coordinating or delivering colonoscopy services we are keen to hear from you!
Opportunities to be involved
We would be grateful for your input on this important research. You can participate by:
and/or
If you are interested in participating, please complete an expression of interest form using the link below.
New Cervical Screening Behaviour Change Campaign now live
A new Cervical Screening Behaviour Change Campaign launches on 3 November 2024, aiming to motivate women and people with a cervix to do the Cervical Screening Test when due.
Cancer Institute NSW’s campaign will run across social media, radio, and paid search, targeting women and people with a cervix in NSW aged 30-50 years in NSW, including Mandarin speaking women, as well as Aboriginal and Torres Strait Islander women and people with a cervix in NSW aged 25-45.
A Cervical Screening Test every five years is the best way to prevent cervical cancer, which kills one in every three women who is diagnosed with the disease. Despite this, only 59% of eligible women and people with a cervix in NSW are doing the test when they are due, down from 63% in 2023.1
There are now two options for doing the test – one is to have a healthcare provider collect a sample, the other is for women to collect their own sample, in private, at a medical centre. Both are equally accurate and effective. The self-collection option is great for patients who might feel anxious or embarrassed about having a clinician collect their sample or who are concerned about potential discomfort associated with the use of a speculum.
For more information on cervical screening visit Cervical screening for health professionals | Cancer Institute NSW
The Cancer Institute NSW is encouraging GPs and primary care professionals across the state to support the campaign by encouraging their patients to do the Cervical Screening Test and offering them the option to collect their own sample.
For more information about the campaign, visit
2024/25 Cervical Screening Campaign | Cancer Institute NSW
1 Australian Institute of Health and Welfare. (2023). Cancer screening programs: quarterly data, Cervical screening participation: https://www.aihw.gov.au/reports/cancer-screening/national-cancer-screening-programs-participation/contents/national-cervical-screening-program/participation Accessed: October 20 2024
November 2024 news and updates
GPs needed to help codesign a new referral tool for colonoscopy!

Primary care practitioners’ referrals for colonoscopy are crucial for enhancing the efficiency and effectiveness of colorectal disease and cancer. Developing a locally relevant decision aids and offering targeted education programs will support informed decisions, improving the accuracy of referrals and optimising the allocation of healthcare resources, especially given the recent update to the clinical practice guidelines.
We are looking for General Practitioners in NSW to contribute to the early development of this project through:
These tasks are occurring between Oct and Dec 2024. We are seeking GPs who would be happy to be involved in discussions with the Daffodil Centre research team over this period. If you are interested or would like further information, please contact Joanna Jaques, Research Program Manager, Gastrointestinal Cancer Policy and Evaluation, on joanna.jaques@sydney.edu.au.
October 2024 news and updates
‘Own It’ & ‘Screen Me’ National Cervical Screening Campaigns
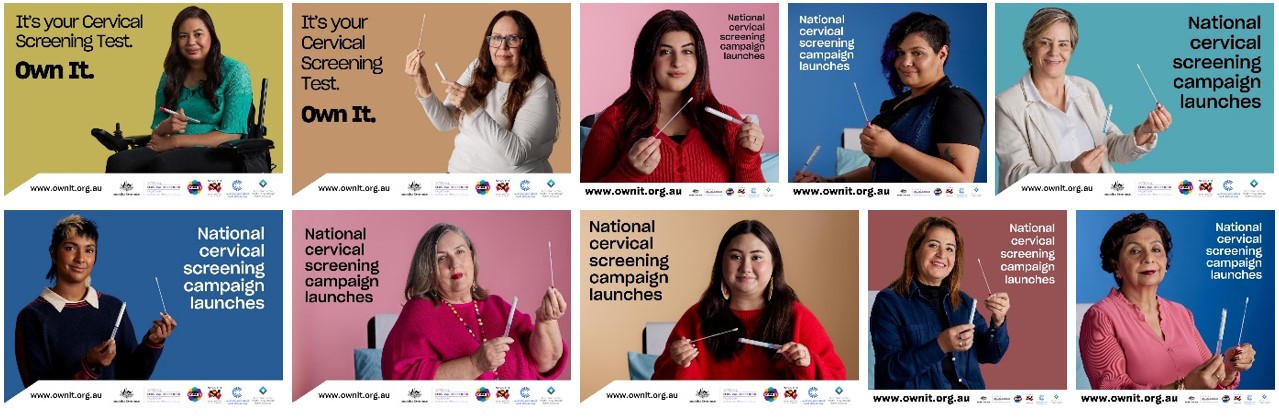
Cervical cancer is highly preventable, and Australia is on track to become the first country to eliminate it. However, this depends on maintaining or increasing screening rates and ensuring that all eligible individuals with a cervix participate.
The ‘Own It’ and ‘Screen Me’ campaigns focus on boosting testing rates among the most under-screened communities, including:
These campaigns may lead to an increase in patients inquiring about cervical screening and the self-collection option.
Learn more about offering choice in cervical screening by visiting (for healthcare providers).
'Own It' is a collaborative effort involving ACON, the Australian Centre for the Prevention of Cervical Cancer, the National Aboriginal Community Controlled Health Organisation, and the Australian Multicultural Health Collaborative (managed by the Federation of Ethnic Communities Councils of Australia). ‘Screen Me’ is a collaboration with Daffodil Centre, Cancer Council/University of Sydney and Centre for Disability Studies.
Learn more about the campaigns by visiting
https://www.health.gov.au/screen-me
October is breast cancer awareness month

GPs and primary care professionals are instrumental in encouraging women to have their regular breast screen.
This October, we urge you to remind women about the importance of early detection of breast cancer and encourage Aboriginal and Torres Strait Islander patients to have a free mammogram every two years from age 40-74.
The breast screening guide for GPs (PDF) has been developed to support you.
You can also download this poster and factsheet for your practice.
Aboriginal and Torres Strait Islander women are less likely to participate in routine breast screening and have poorer outcomes than non-Aboriginal women in relation to surviving a breast cancer diagnosis. A comprehensive toolkit for the Aboriginal health workforce has been developed to support communities to live healthy.
September 2024 news and updates
National Bowel Cancer Screening Community Roadshow
The National Bowel Cancer Screening Program’s ‘Get behind it’ community roadshow is on the road visiting towns in metro and regional NSW throughout August and September 2024.

As part of the Australian Government’s ‘Get Behind It’ campaign, the National Bowel Cancer Screening Program community roadshow will be visiting towns in NSW this August and September.
The National Bowel Cancer Screening Program is a free Australian Government program that aims to reduce bowel cancer deaths through early detection. People aged 45 to 49 can now request their first free kit and join the program. People aged 50 to 74 will continue to automatically receive their kit every two years.
Since June 2024, the team have been on the road with their trailer stopping in towns across the country to give communities life-saving information on this free program. Some of the towns they’ve visited so far include Darwin, Katherine, Alice Springs, Cairns, Innisfail, Ayr and Townsville.
The team will be stopping in the following NSW towns on the dates listed (with some specific locations to be confirmed and being identified with local councils, clubs and businesses).
Sydney
Regional NSW
For further information, watch this video featuring Dr Andrew Rochford. To support events in your local area you may wish to:
National Lung Cancer Screening Program set to Launch in July 2025
Earlier this year the Australian Government announced the implementation of a National Lung Cancer Screening Program (NLSCP), set to launch in July 2025.
The NLSCP presents a significant opportunity to increase early diagnosis, enhance treatment options and improve survival for one of the deadliest cancers in NSW. It will use low-dose CT scans to look for lung cancer in high-risk people without any symptoms.
Your patients will be eligible for the new screening program if they:
and
or
Two new Medicare Benefit Schedule (MBS) items will be created to provide low-dose computed tomography (LDCT) scans under the NLCSP. The new MBS items are for:
Your practice can begin to prepare for implementation in the following ways:
The NLSCP will be led by the Commonwealth Government, with support from states and territories. For more information visit the Commonwealth Government website.
August 2024 news and updates
Have your say: education needs for the upcoming National Lung Cancer Screening Program

A National Lung Cancer Screening program is being implemented in July 2025, providing lose dose CT (LDCT) scans to people aged 50-70 years with a 30 pack year history of smoking.
The Cancer Institute NSW is working with the Commonwealth, LHDs, PHNs and the AH&MRC to plan and support the implementation of the program into NSW. This includes modelling the expected activity for the program, mapping current CT capacity in NSW, and determining the areas of need in regional areas for a mobile CT service to be delivered.
University of Melbourne is developing the NLCSP Program guidelines and has been consulting with key stakeholders nationally to do this, under the guidance of a clinical advisory committee.
A new research project called “Design of information content for the National Lung Cancer Screening Program”, seeking to help identify and clarify the education and information needs for the National Lung Cancer Screening Program in Australia. This study is funded by Cancer Australia and is being conducted by a team of researchers at The Daffodil Centre.
The project team are seeking people who are:
Participation would involve a 30-60minute interview in the next few weeks, with additional consultation opportunities over the next few months. Taking part in some or all the consultation activities is voluntary, and you will be offered a $50/hour gift voucher for taking part.
If you are interested in participating, please complete an Expression of Interest form.
Bowel Cancer Screening Program: Eligibility age lowering and alternative access to kits for healthcare providers
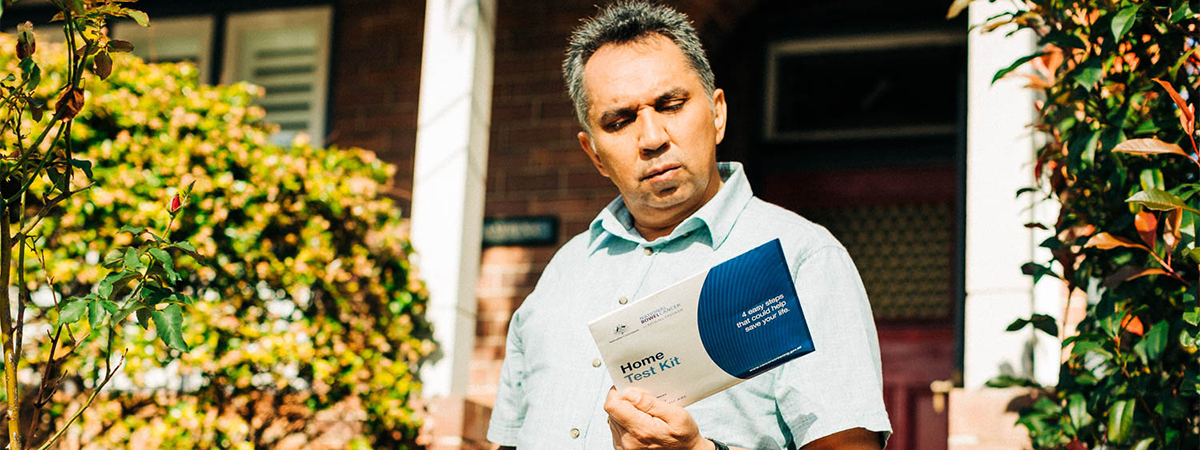
The Government has announced that from 1 July 2024 it is lowering the eligible screening age for the National Bowel Cancer Screening Program from 50 to 45. This means that people aged 45 to 49 can now join the National Bowel Cancer Screening Program by requesting their first free bowel cancer screening kit from the NCSR or by calling the Contact Centre on 1800 627 701.
Eligible people aged 50 to 74 will continue to receive a bowel cancer screening kit in the mail every 2 years automatically.
People aged 45 to 74 can also ask their doctor about getting a kit. Healthcare providers can bulk order program kits and issue them to eligible patients via the Program’s alternative access to kits model.
Patients are more likely to do the test when it has been discussed with a trusted healthcare professional. Healthcare providers are in a unique position to encourage people who have never screened, or are overdue for screening, to take that positive next step towards bowel cancer screening. Offering an eligible patient a program kit means they are supported by the National Bowel Cancer Screening Progam, including invitations and reminders to screen, and follow up of every participant with a positive test by a dedicated team to ensure they see their GP and are encouraged to go on to have a colonoscopy where the GP has deemed it appropriate.
To get started with offering NBCSP kits, visit the link below to do the training and bulk order kits for your practice.
Further resources:
Do the Test - Cancer Institute NSW
National Bowel Cancer Screening Program
How to do the test instructions
Order demonstration bowel screening kits
GPs needed for feedback around improving colonoscopy referrals
Throughout July 2024, GPs can go to this link to complete a short survey about their experiences of referring patients for colonoscopy after a positive bowel cancer screening test (also known as an immunochemical faecal occult blood test or iFOBT).
The objectives of the survey and interviews are to:
Please share this invitation with GPs and encourage them to complete the survey so they can have their say on this important area of cancer screening.
NEW GP cancer screening kits with translated materials
In 2022 the Australian Government distributed GP cancer screening engagement packs to over 7000 general practices across Australia including demo bowel screening kits, cervical screening swabs and waiting room posters. As part of the evaluation of this initiative, GPs indicated that the packs were valuable and that future kits should include translated resources for people from culturally and linguistically diverse communities. As a result, the Government will be mailing updated kits to practices, which will include multicultural resources to further assist GPs with encouraging patients to screen for bowel, breast, and cervical cancer.
The updates packs will include:
Digital copies of the printed materials can also be found on the Department of Health and Aged Care website.
July 2024 news and updates
New Lung Cancer Screening Program website and resources now live!
The new National Lung Cancer Screening Program aims to reduce deaths from lung cancer by facilitating early detection in high-risk individuals. Screening services will begin in July 2025. To provide healthcare providers and participants with important information about the upcoming program, the Australian Government Department of Health and Aged Care (DHAC) has launched a National Lung Cancer Screening Program website. The new website includes information on:
The website will be regularly updated with new information as design and implementation planning for the program continues.
A National Lung Cancer Screening program is being implemented in July 2025, providing lose dose CT (LDCT) scans to people aged 50-70 years with a 30 pack year history of smoking.
The Cancer Institute NSW is working with the Commonwealth, LHDs, PHNs and the AH&MRC to plan and support the implementation of the program into NSW. This includes modelling the expected activity for the program, mapping current CT capacity in NSW, and determining the areas of need in regional areas for a mobile CT service to be delivered.
University of Melbourne is developing the NLCSP Program guidelines and has been consulting with key stakeholders nationally to do this, under the guidance of a clinical advisory committee.
A new research project called “Design of information content for the National Lung Cancer Screening Program”, seeking to help identify and clarify the education and information needs for the National Lung Cancer Screening Program in Australia. This study is funded by Cancer Australia and is being conducted by a team of researchers at The Daffodil Centre.
The project team are seeking people who are:
• Members of the primary care workforce
• Specialists with a direct role in the National Lung Cancer Screening Program
• Members of professional colleges and peak bodies relevant to lung cancer screening
Participation would involve a 30-60minute interview in the next few weeks, with additional consultation opportunities over the next few months. Taking part in some or all the consultation activities is voluntary, and you will be offered a $50/hour gift voucher for taking part.
If you are interested in participating, please complete an Expression of Interest form.
Express Interest
‘HPV Self-Collection: Are YOU ready to support the choice?’
In recent years, the National Cervical Screening Program has seen substantial transformations, notably with the implementation of universal access to HPV self-collection. This method stands out as one of our most effective tools for enhancing screening participation and advancing toward the equitable elimination of cervical cancer in Australia.
HPV self-collection allows screening participants to take their own vaginal sample for HPV testing. It is just as sensitive for the detection of CIN2+, adenocarcinoma in situ, and oncogenic HPV as a clinician-collected cervical screening test via a speculum examination and is available as an option for all routine (asymptomatic) participants in the National Cervical Screening Program. Self-collection is one of the best tools we have available to increase cervical screening participation, address disparities in screening, and keep us on track to eliminate cervical cancer in Australia by 2035.
In September 2024, the Australian Government will be funding a consumer facing campaign around national cervical screening – the first of its magnitude in over 20 years. In advance of this campaign, the Australian Government Department of Health and Aged Care has funded the Australian Centre for the Prevention of Cervical Cancer to undertake a nationwide healthcare provider awareness campaign, ‘HPV Self-Collection: Are YOU ready to support the choice?’. The materials for this campaign were developed in partnership with The National Aboriginal Community Controlled Health Organisation (NACCHO) and the Australian Multicultural Health Collaborative (AMHC). The campaign aims to encourage healthcare providers to ensure their practices are ready to offer the HPV self-collection option to all who are eligible in advance of the patient-facing campaign.
Find resources, CPD online learning modules, videos, and information on how to support under-screened groups at the campaign website.
Further resources:
You can:
June 2024 news and updates
What is your local bowel cancer screening participation rates? Share our Bowel Screening QI module for Bowel Cancer Awareness month.
Bowel cancer is Australia’s second deadliest cancer, but if detected early, bowel cancer can be successfully treated in more than 90% of cases. Primary care teams are instrumental in supporting prevention, encouraging informed screening participation and facilitating pathway progression for the earliest possible diagnosis of bowel cancer.
In support of this, the Cancer Institute NSW has developed a Primary Care Cancer Control Quality Improvement Toolkit in consultation with the primary care health sector. The Toolkit includes a bowel screening quality improvement (QI) module which is filled with practical information and resources to guide general practices and health services to enhance local bowel cancer screening participation.
Head to our Toolkit now and share our module with your primary care networks in time for Bowel Cancer Awareness month in June!
May 2024 news and updates
NEW BreastScreen NSW website with easy breast screening booking and health professional resources
BreastScreen NSW has launched a brand-new website which offers useful resources for health professionals. It plays a crucial role in raising awareness about the program, facilitating easy access to screening information and encouraging a seamless screening booking process.

BreastScreen NSW has launched a new website which provides improved functionality, better navigation and updated health professional and consumer facing information on breast screening. It aims to contribute to an increase in breast screening bookings. Some of the new features include:
The website primarily targets women in NSW aged 50–74, but it also caters for the audiences below:
Support the launch
You can support the launch by sharing our:
For more information about the new website, reach out to our BreastScreen NSW team at CINSW-BreastScreenNSW@health.nsw.gov.au.
Catch up on the latest RACGP and Cancer Institute NSW Webinar!
The Cancer Institute NSW recently partnered with the RACGP to deliver a 1-hour educational webinar on how to locally tailor and enhance cancer prevention and screening activities. Watch the recording for NSW cancer data insights and an overview on how to use the Institute’s Primary Care Cancer Control Quality Improvement Toolkit.

This 1-hour educational webinar provides guidance for primary care teams, through reflective practice, to enhance cancer prevention and support informed participation in the national cancer screening program. The panellists outline relevant NSW cancer data insights and provide an introduction of the Institute’s Primary Care Cancer Control Quality Improvement Toolkit for use in practice.
The webinar was delivered by the Institute and A/Prof Carolyn Ee, a Survivorship Specialist, Supportive Care & Integrative Oncology Specialist GP at the Chris O’Brien Lifehouse and Scientific Committee Member at the Primary Care Collaborative Cancer Clinical Trials group.
Webinar learning outcomes:
February 2024 news and updates
Swab the Facts: Cervical Screening Self-Collection
Since cervical screening self-collection became universally available across Australia in 2022, healthcare providers have had recent and never screened patients asking for the new test and seeking advice on how it all works.
From the evidence and experience, we already know the following key points about self-collection:
Clinics offering cervical screening self-collection have processes and instructions in place based on the type of swabs they use and where that type of swab is being processed across Australia. Noting on the Pathology Request form that the test was self-collected is essential AND correct labelling of these swabs with details of the specimen and swab type is a crucial step that makes a big difference.
Dry swab accredited labs (Copan 552C/Copan 5E089N) include:
Roche-validated labs for Copan 552C.80 swabs in NSW include:
Healthcare providers in cervical screening are speaking to their usual Pathology Laboratory providers to understand the specifics of the swabs they use - we cannot afford to have previously under, or never-screened women finally feel empowered to test themselves, only to return an unsatisfactory result from the laboratory as it was not collected correctly!
BreastScreen Australia – Public consultation NOW OPEN
The Commonwealth in partnership with state and territory governments, is undertaking a review of the BreastScreen Australia Program.

The BreastScreen Australia Review (the Review) will inform the future strategic direction of BreastScreen Australia, and consider emerging evidence and research, safety and quality, funding models and maximising equity and participation.
The review will develop evidence-based recommendations to improve the BreastScreen Australia Program. These recommendations will guide the strategic direction of the program and support measures that:
The review will also consider recommendations from the Roadmap for Optimising Screening in Australia as well as broader program considerations including the funding model and quality and safety mechanisms.
The Commonwealth are seeking your views. Public consultation as part of the review is now open on the Department’s Consultation Hub until 20 February 2024, or, linked here.
Pregnancy and cervical screening: Everything GP Shared Care Program providers need to know
To optimise cervical screening implementation within GP Antenatal Shared Care Programs, a new PowerPoint resource has been developed for presentation in ANSC Committee meetings. This resource ensures consistent messaging on the safety and benefits of cervical screening during pregnancy among all collaborating practitioners involved in pregnancy care.
Cervical screening is safe at any time during pregnancy. For some women, pregnancy may be the first time they are offered cervical screening, especially those women who are not regularly connected with health services. Cervical screening is for all women and people with a cervix from 25-74 years of age who have ever been sexually active.
Pregnancy is an opportune time for women to receive important health information, with more frequent healthcare visits and a focus on maternal health. Routine antenatal and postnatal care should include cervical screening history and a Cervical Screening Test if a woman is due.
During pregnancy care, women may see many different healthcare providers. Within the GP Antenatal Shared Care Program model of care, pregnancy care is shared between GPs and midwives and doctors from the hospital antenatal clinic. Providing consistent information is vital so that women feel confident and supported to make informed decisions about their healthcare.
The NSW Cervical Screening Program has developed a new resource, in collaboration with the Cervical Screening During Pregnancy Project Working Group, to provide up-to-date cervical screening information to all healthcare providers who work with women during pregnancy care. Information includes:
The resource is designed to be presented at Antenatal Shared Care Program Committee meetings or information sessions to ensure that the range of healthcare providers who work with women are equally aware of the safety and importance of cervical screening during pregnancy, including the choice between self-collection or clinician-collection for a Cervical Screening Test sample, and any follow up that may be required. This will help to ensure that all pregnant women are asked about and offered cervical screening during their pregnancy and can make an informed choice to have cervical screening during pregnancy with the appropriate provider.
The resource is available to download from the Cervical Screening During Pregnancy webpage.
Please find out more about cervical screening during pregnancy on our website.
- The mobile CT screening service commence in 2027.
- CINSW continues to meet with the Commonwealth, Heart of Australia and other jurisdictions to finalise route planning.
- For more information about breast density and breast density reporting visit www.breastscreen.nsw.gov.au/professionals
- Women are more likely to have a mammogram if it is recommended by their GP. To make an appointment at a local BreastScreen NSW clinic or mobile van, call 13 20 50 or book online at www.breastscreen.nsw.gov.au
- Perform guideline appropriate assessment and management of colorectal cancer risk.
- Perform guideline appropriate assessment and triage for colonoscopy.
- Generate guideline appropriate referral for colonoscopy services, including use of Direct Access Colonoscopy (DAC) services in NSW.
- The timing to deliver Heart of Australia mobile CT services for states and jurisdictions is still being negotiated. There is delayed commencement of mobile service until 2027.
- CINSW continues to meet with the Commonwealth, Heart of Australia and other jurisdictions to finalise van allocation and considerations for route planning.
- CINSW, with support from Ministry of Health's Nursing and Midwifery office, has submitted a response to a review of the Nurse Practitioner role in the NLCSP.
- This role supports the NLCSP, including requesting a LDCT. The Commonwealth is considering authorisation of NPs as requesting providers for LDCT.
- Led by University of Melbourne, ‘Ready to Screen’ aims to identify the most effective strategies for engaging eligible patients to take up lung cancer screening.
- The trial will understand how communication from a patient’s general practice can increase participation rates, how practices can be better supported to deliver the NLCSP, and barriers/enables to implementing the program.
- For more information, email ready-to-screen@unimelb.edu.au or call 0459 867 617.
-
Be supported to identify patients who may be eligible for screening.
-
Gain access to Future Health Today, a point-of-care clinical decision support tool, integrated into your existing software.
-
Receive a list of patients interested in being contacted for eligibility assessment.
-
Be supported onsite by one of our research nurses.
-
Receive $2000 AUD reimbursement for your time, with your clinical staff eligible to claim up to 4.5 continuing professional development (CPD) hours for participation.
-
Have at least two full-time equivalent GPs and a practice manager (or delegate).
-
Use electronic medical record (EMR) software (e.g., Best Practice, Medical Director, ZedMed) and be able to extract patient cohort lists.
-
Have the ability to send SMS reminders to patients.
- 2-page Quick Reference guide - cervical screening
- NCSP summary guide for healthcare providers
- Understanding the NCSP Management Pathway: A guide for Healthcare Providers
- Updated healthcare provider education and training modules are available on the Australian Centre for the Prevention of Cervical Cancer (ACPCC) website. There are 5 free interactive eLearning modules in line with the updated guidelines and is CPD accredited with RACGP & ACRRM.
- The Royal Australian College of General Practitioners (RACGP) educational webinars - 2025 cervical screening update: what you need to know about the latest guidelines are scheduled for:
- completing a short online survey
- taking part in a 45-minute interview with the Nous team
- Supporting a needs assessment and development of learning outcome and preliminary content for a colonoscopy education module, which are aligned with General Practice needs (to support subsequent RACGP accreditation)
- Co-design of a decision aid tool for referrals to colonoscopy
- Aboriginal and/or Torres Strait Islander women
- Women from multicultural and diverse backgrounds
- Sexually and gender diverse people
- Women living in rural and remote areas
- Women with disabilities
- Sydney CBD Thursday 29 August
- Blacktown Friday 30 August – BlueBet Stadium ‘Panthers vs Rabbitohs’
- Campbelltown Saturday 31 August – MarketFair Campbelltown
- Queanbeyan Wednesday 4 September – The Roos Club
- Lake Macquarie Monday 9 September
- Newcastle Tuesday 10 September
- Wednesday 11 September
- Port Stephens Thursday 12 September
- Port Macquarie Saturday 14 September – Marine Rescue and Glasshouse Port Macquarie
- Tamworth Monday 16 September – Tamworth Shopping World
- Tuesday 17 September – Tamworth Bunnings
- Narrabri Thursday 19 September – Narrabri Bunnings
- Bourke Saturday 21 September – Bourke District Hospital
- Dubbo Tuesday 24 September – Dubbo Bunnings
- Check their events page for regular updates on locations
- Follow the roadshow on Facebook and Instagram and re-share posts promoting your local events
- are aged between 50 and 70 years
- show no signs or symptoms of lung cancer
- have a history of at least 30 pack-years of cigarette smoking and are still smoking
- have a history of at least 30 pack-years of cigarette smoking and quit in the past 10 years.
- The screening LDCT scan done by the participant every 2 years.
- The interval LDCT scans for any follow-up needed during the 2-yearly screening period (as required following results of the screening LDCT test).
- Consider how you might be able to reach patients eligible for the new screening program.
- Review your databases to:
- Identify patients who currently smoke or who have quit smoking and are between the ages of 50 and 70.
- Ensure information about your patient's smoking status and history are complete and accurate.
- Confirm your integration with the National Cancer Screening Register.
- Members of the primary care workforce
- Specialists with a direct role in the National Lung Cancer Screening Program
- Members of professional colleges and peak bodies relevant to lung cancer screening
- Understand and describe general practitioners’ current referral pathways to colonoscopy.
- Gather general practitioners’ perspectives on Direct Access Colonoscopy (DAC) services in NSW, including perceived barriers, enablers, benefits, and other consequences of the services.
- Identify the determinants (including barriers and facilitators) that may impact the use of DAC in NSW.
- Identify focus areas for improvement and implementation interventions/behaviour change strategies to increase use of DAC services by general practitioners with eligible +iFOBT patients in NSW.
- A3 posters, one for each national cancer screening program, with reminder messaging and information on how to book. Practices are encouraged to hang these in waiting rooms and other high traffic areas to prompt conversations about cancer screening. Translations of the poster in over 20 languages are available to be printed in-practice.
- Demonstration samples of the bowel cancer screening home test kit and the cervical screening self-collection swab to show patients how to do the tests.
- Illustrated infographics on how to use the cancer screening tests and where to find educational resources on cancer screening. Translations of the illustrated guides are available in over 20 languages online.
-
The important role of healthcare providers and the support available to ensure successful delivery of the program
-
Eligibility criteria and how to calculate pack year history,
-
How the screening program will work
-
Key information including details about Program guidelines, MBS items for Low Dose CT scans, reporting requirements and how to access the National Cancer Screening Register
-
Ongoing work to ensure that the screening program will be equitable, accessible and culturally safe
-
The program’s governance framework, including advisory bodies, clinical and jurisdictional representation, and contacts for the DHAC .
-
Sign up for a webinar about self-collection.
-
Complete CPD accredited online learning modules.
-
Download provider clinical resources, as well as patient resources.
-
Contact your laboratory to ensure you have the correct swabs and instructions to offer self-collection.
-
Remember that self-collection is just as sensitive for the detection of HPV and CIN2+/adenocarcinoma in situ as a clinician-collected cervical sample and can be offered to all cervical screening patients.
-
Understand barriers for under-screened groups and how provider cultural competence and the option of self-collection can overcome them.
-
Ensure you feel confident supporting patients to choose what’s right for them
- An improved location finder, so it’s never been easier to find out where you can screen that’s convenient for you.
- A mobile-first design, ensuring ease of use for women accessing the site on their devices.
- Improved access to the booking page, helping women to easily secure an appointment.
- Updated content for communities, including Aboriginal and multicultural women, improving engagement and accessibility. The site has translation in three languages with more languages planned for the coming year.
- An expansive FAQ section, answering common questions about the screening process
- Aboriginal women aged 40–74 in NSW
- Culturally and linguistic diverse women aged 50–74, with a focus on Chinese, Vietnamese and Arabic languages (and supported by a key resource that is translated in 27 languages)
- Health professionals
- Women with a disability or special need
- Women in rural or remote areas
- Trans and gender diverse people
- Women of all ages wanting to find out more about breast screening
- Friends and family of screening women
- Outline current NSW performance and trends in cancer prevention and screening
- Identify key elements underpinning team-based, cancer focused, quality improvement in the practice setting
- Outline data and systems utilisation to support participation in national cancer screening and preventive programs to reduce cancer risk
- Summarise a Patient-centred approach to tailored information and care that is responsive to people’s individual needs and preferences
- Same Accuracy, New Approach: Evidence shows equivalent sensitivity for HPV tests on self-collected vaginal samples and clinician-collected cervical samples, using PCR-based tests as recommended by the National Cervical Screening Program.
- HPV Focus, Simplified Process: Self-collection tests solely focus on HPV, meaning no more cell scraping. It is a simple vaginal swab, offering a comfortable and private alternative.
- As this process does not collect samples from the cervix, a small number of women with a positive HPV result will have to return for a clinician-collected test (liquid-based cytology) or referred for colposcopy.
- No DIY Kits: Commercially available self-collection kits are not available in Australia for primary screening. Accreditable pathology labs process all samples using one of three approved swab types.
With three self-collect swabs currently available in Australia, it important to know the difference in processing.- Copan 552C (dry) swab is transported dry to accredited labs for processing.
- Copan 552C.80 swab is for use with the Roche device. The swabs must be immediately suspended in ThinPrep solution and the ThinPrep vial sent to Roche verified labs for processing.
- Copan 5E089N swab is for use with the Becton Dickinson (BD) device. These swabs can be transported dry to BD verified labs for processing.
- Victorian Cytology Service Pathology
- Sonic labs
- Clinipath
- Douglas Hanly Moir Pathology
- Sullivan Nicolaides Pathology
- Melbourne Pathology
- NSW Health Pathology - John Hunter, Pathology North
- Laverty Pathology
- Douglas Hanley Moir Pathology
- enable a nationally consistent approach to breast screening practices
- increase program participation
- improve the participant experience
- make the service more efficient and productive.
- Cervical screening, HPV, and cervical cancer
- Self-collection
- Results and management
- Cervical screening during pregnancy, including case study.
- National Cervical Screening Register
- Resources and links to more information
2023 program news and updates
New online toolkit available - Helping Mob Live Healthy and Prevent Cancer toolkit for health professionals
Aboriginal people in NSW experience a higher burden of cancer than other groups. The Cancer Institute NSW is committed to improving cancer outcomes and supporting culturally safe, tailored cancer care for the Aboriginal community.
This month, the Institute is proud to launch a new online toolkit, Helping Mob Live Healthy and Prevent Cancer. This is ‘one-stop shop’ hub of information for health professionals caring for Aboriginal clients – including GPs and other staff in the primary care sector.
The Helping Mob Live Healthy and Prevent Cancer toolkit features:
- cancer screening information – breast, cervical and bowel cancer screening
- cancer prevention tips about healthy living and wellness for Aboriginal people
- downloadable resources for Aboriginal people, which can be used to support yarns with your clients about the benefits of taking part in cancer screening and healthy living.
All resources have been developed in consultation with Aboriginal health organisations and community members. Resources are designed to appeal to Aboriginal people, and take a strengths-based, culturally tailored approach.
The goal of the Helping Mob Live Healthy and Prevent Cancer toolkit is to educate and empower Aboriginal people to reduce their cancer risk – and ultimately contribute towards reducing cancer rates and increasing positive health outcomes for Aboriginal people in NSW.
We encourage you to visit the toolkit, share and circulate it to your networks, and like and share our social media posts and promotional materials.
BreastScreen NSW has launched a new campaign
Breast cancer is the most common cancer affecting women in NSW, with 1 in 7 women developing breast cancer in their lifetime. In 2020 alone, breast cancer claimed the lives of 1,024 women in the state.
Despite this, more than 620,000 NSW women in the target age group of 50–74 years have not had their recommended breast screen in the past two years.
Research has found that many women are not prioritising their health amidst the busyness of their lives and therefore do not participate in regular breast screening. In response to this, the Cancer Institute NSW has developed the new campaign to motivate women aged 50–74 in NSW to book a breast screen when due.
GPs and primary care professionals are instrumental in encouraging women to have their regular breast screen.
A breast screening guide for GPs (PDF) has been developed to support this process.
This October, we urge you to remind women about the importance of the early detection of breast cancer and recommend they book in for their free mammogram.
View the campaign toolkit online. To support the campaign:
- Circulate the toolkit among your staff and networks
- Like and share our campaign social media posts
- Print our posters and display prominently
To book an appointment call 13 20 50 or book online.
Promoting BreastScreen NSW to your patients post-Covid
Breast cancer is the second most common cancer in NSW and one in seven women will develop breast cancer in their lifetime. Regular two-yearly breast screening remains the most effective method of detecting breast cancer in its early stages. Breast cancer survival rates are as high as 98% if detected early.
Breast screening rates were impacted by the COVID-19 pandemic resulting in patients delaying their regular screen or not screening at all.
- In response to the first wave, BreastScreen NSW temporarily suspended screening services on 27 March 2020, recommencing services by 18 May 2020. In 2020 the number of screens were 16% lower compared to 2019.
- In response to the second wave, BreastScreen NSW progressively suspended services from June 2021, with all services closed from 19 August 2021 and all were operational again by 22 November 2021. There were 25% fewer screens in the January to November period compared to the equivalent period in 2019.
BreastScreen NSW is fully operational and has contacted all women impacted by closures urging them to book in for their routine mammogram.
Research from BreastScreen NSW shows that General Practitioners have a significant influence on a woman’s decision to have a screening mammogram. Although a referral is not required to attend the BreastScreen NSW program, GPs and practice nurses play an important role in providing support and encouragement to patients to participate, as your patient is more likely to have a breast screen if you recommend it to them.
- This Guide (PDF) provides information for GP's about BreastScreen NSW.
- Encourage your patients to use this free service and book online through our website: book.breastscreen.nsw.gov.au or by calling 13 20 50.
- Free promotional resources for your practice can be ordered from BreastScreen NSW.
- Access the Breast Screening Module within Primary Care Cancer Control Quality Improvement Toolkit to learn more about QI activities that provide a patient centred approach to increase breast screening participation in your practice, while earning CPD points.
A free, 20-minute breast screen could save your patients life.
For more information, please contact your local BreastScreen NSW service on 13 20 50.
Receive continuous professional development points from the quality improvement toolkit

The Primary Care Cancer Control Quality Improvement Toolkit is an easy-to-follow roadmap for improving cancer screening and prevention activities in your practice or health service.
Each module provides guidance for steps required to promote patient-centred care and guide a team-based approach to quality improvement, utilising data and systems to increase participation in national cancer screening programs and preventive programs to reduce cancer risk.
On completion, five continuous professional development hours of self-directed learning can be claimed by documenting your learning and activities. See an example template from AHPRA here (under Appendix 1).
Jump to:
- World Refugee Day - 20 June 2023
- Direct Access Colonoscopy Services in NSW
- Offering bowel cancer screening to your patients just got easier
World Refugee Day - 20 June 2023
World Refugee Day allows us to celebrate the resilience of people from a refugee background and reflect on how we can support them to ‘not only survive but also thrive’.1
Many refugee patients that you see have been forced to flee their home and are at various stages of rebuilding their lives in a new country. ‘GPs are often the first and main point of contact between refugees and the healthcare system’.2
Preventive health measures like cancer screening will be unfamiliar to some people from refugee backgrounds and should be explained.3
Recent consultations by the Cancer Institute NSW and partners found that people from refugee backgrounds said they would be motivated to screen if their GP had a conversation with them. People said an explanation from their GP would help them to understand the importance of screening and feel comfortable completing screening tests.4
Conducting MBS-covered Refugee Health Assessments is encouraged and would allow time to discuss and explain cancer screening to new patients.
The Australian Refugee Health Practice Guide recommends that you offer a Refugee Health Assessment to ‘every child, adolescent and adult from a refugee background who is new to your care’.5
This Refugee Health Assessment template is endorsed by the RACGP and published by Victorian Refugee Health Network.
More information:
- Learn more about World Refugee Day
- Refugee Health Assessment template - endorsed by the RACGP
- Refugee Health Assessment guide in the Australian Refugee Health Practice Guide
- Health Professional information from NSW Refugee Health Service
Sources:
1. UNHCR
2. SWSLHD - NSW Refugee Health Services
3. SWSLHD - NSW Refugee Health Services
4. [unpublished] Data derived from 17 focus group conversations with 161 people from the Refugee Cancer Screening Project, Cancer Institute NSW.
5. refugeehealthguide.org.au
Direct Access Colonoscopy Services in NSW
Direct Access Colonoscopy (DAC) is a NSW Health Leading Better Value Care initiative that focuses on improving timely access to public colonoscopy services following a positive bowel cancer screening test. DAC services aim to reduce barriers commonly faced by patients including:
- extended wait times for colonoscopy
- unnecessary face-to-face outpatient clinic appointments
- time spent travelling to specialists/outpatient appointments
- out-of-pocket costs for private specialist room appointments.
A DAC service aims to mitigate the impact of these barriers by allowing clinically eligible patients to be assessed over the telephone by a Clinical Nurse Consultant. A nurse-led telephone triage assessment enables patients meeting the inclusion criteria to be referred directly to a DAC service, while also allowing specialist clinic time to be directed to more complex patients. DAC services require a well-structured and protocolised triage and assessment pathway which assures safe, independent assessment by nursing staff with specialist oversight.
In 2022, a process evaluation was undertaken aimed at understanding the extent to which implementation of DAC has progressed as planned and to identify potential achievements against expected short-term outcomes.
Key enablers to implementation included executive buy-in, having the right people in roles at the right time and support and guidance from the Cancer Institute NSW.
Key barriers to implementation included the existence of alternative services, lack of funding/resourcing, and impacts of the COVID-19 pandemic. Most services reported high levels of engagement with primary care, although there are opportunities for increased engagement in view of COVID-19 impacts easing.
There are currently 19 DAC services across NSW, with plans for further services in development.
General practitioners (GPs) can refer their patients to a local DAC service via their local Health Pathways portal.
The table below outlines the available DAC services in NSW.
| Primary Health Network (PHN) | DAC Service available at: |
| Central and Eastern Sydney | |
| Hunter New England and Central Coast | |
| Murrumbidgee | Cootamundra |
| Nepean Blue Mountains | Blue Mountains Hospital |
| North Coast | Coffs Harbour |
| Northern Sydney | Ryde |
| South Eastern NSW | Queanbeyan |
| South Western Sydney | |
| Western NSW | |
| Western Sydney |
Offering bowel cancer screening to your patients just got easier
Bowel cancer is Australia’s second biggest cancer killer.
Yet, it’s also one of the most treatable cancers, with more than 90% of cases successfully treated if found early.
A late-stage bowel cancer diagnosis does not have the same positive outcomes, so encouraging eligible people to screen every two years is key.
The bowel screening test is accurate, cost effective, non-invasive, and is the front line for bowel cancer screening in people who are asymptomatic or at average-risk. It is a simple test that is done at home. It looks for invisible traces of blood in poo, which could be a sign of cancer or a pre-cancerous growth.
General practitioners can now hand out kits
We know that patients are more likely to do the test when it has been discussed with a trusted healthcare professional who can explain how to do the test and why it is important.
Encouraging your patients aged 50 to 74 to screen for bowel cancer just got easier, with the National Bowel Cancer Screening Program now enabling healthcare providers to bulk order program kits and to hand kits to eligible patients. It is critical that all kits handed to patients are recorded in the National Cancer Screening Register. This ensures results are tested, sent to the correct address, along with other automated functions such as invitations and reminders to screen.
Please note: the National Bowel Cancer Screening Programs current mailout model will continue in parallel.
How to get started in your practice
Visit the National Bowel Cancer Screening Program’s website to learn more about getting started with the alternative access to kits model.
BreastScreen NSW quick reference guide for primary care
BreastScreen NSW has developed a quick reference guide for General Practitioners and Practice Nurses about routine breast screening.
General Practitioners and Practice Nurses play an important role in providing support and encouragement for patients to participate in the BreastScreen NSW program.
This infographic highlights eligibility and the screening and assessment pathway, and the new recommended screening age for Aboriginal women.
Update of the cervical screening webpages
The cervical screening webpages on the Institute’s website have been revamped and updated to include the most recent information about cervical screening.
Women are more likely to undertake cervical screening at the recommendation of their health professional, or if their health professional has discussed screening with them.
There is a section dedicated to health professionals that includes information about supporting your patients in cervical screening, self-collection key messages and cervical screening during pregnancy.
View the updated section for health professionals >
Direct Access Colonoscopy (DAC) Services in NSW
Direct Access Colonoscopy (DAC) is a NSW Health Leading Better Value Care initiative that focuses on improving timely access to public colonoscopy services following a positive bowel cancer screening test called an immunochemical faecal occult blood test, or iFOBT.
DAC services aim to reduce barriers commonly faced by patients including:
- extended wait times for colonoscopy;
- unnecessary face-to-face outpatient clinic appointments;
- time spent travelling to specialists/outpatient appointments;
- out-of-pocket costs for private specialist room appointments.
A DAC service aims to mitigate the impact of these barriers by allowing clinically eligible patients to be assessed over the telephone by a clinical nurse consultant, rather than attending a face-to-face appointment with a specialist. A nurse-led telephone triage assessment enables patients meeting the inclusion criteria to be referred directly to a DAC service, whilst also allowing specialist clinic time to be directed to more complex patients.
DAC services require a well-structured and protocolised triage and assessment pathway which assures safe, independent assessment by nursing staff with specialist oversight. The service also enables direct colonoscopy booking for patients meeting the inclusion criteria.
There are currently 19 DAC services across NSW, with plans for further services in development.
General Practitioners (GPs) can refer their patients to a local DAC service via their local HealthPathways portal. In most cases, districts have developed a specific DAC referral form and localised inclusion criteria for GPs to use.
The table below outlines the available DAC services in NSW.
| Local Health District (LHD) | DAC Service available at: |
| Central Coast LHD | Gosford Hospital |
| Far West LHD | Broken Hill |
| Hunter New England LHD | John Hunter Hospital |
| Illawarra Shoalhaven LHD | In development |
| Murrumbidgee LHD | Cootamundra |
| Mid North Coast LHD | Coffs Harbour |
| Nepean Blue Mountains LHD | Blue Mountains Hospital |
| Northern Sydney LHD | Ryde |
| South Eastern Sydney LHD | St. George and Sutherland |
| South Western Sydney LHD | Liverpool |
| Southern NSW LHD | Queanbeyan |
| St Vincent's Hospital Network | Darlinghurst |
| Sydney LHD | Camperdown (RPA) and Concord |
| Western NSW LHD | Orange and Dubbo |
| Western Sydney LHD | Blacktown and Westmead |
For further information please contact Alexandra Crocker, DAC Project Implementation Lead Alexandra.Crocker@health.nsw.gov.au.
Biennial screening mammography recommended for Aboriginal and Torres Strait Islander women aged 40–74 years


BreastScreen NSW aims to reduce morbidity and mortality from breast cancer through early detection.
BreastScreen NSW is delivering a pilot, PUTUWA: The BreastScreen NSW Aboriginal women age project, and is now recommending that Aboriginal and Torres Strait Islander women screen every two years from age 40–74.
Breast cancer is the most diagnosed cancer in Aboriginal women and the second most common cause of death. Aboriginal women are less likely to participate in routine breast screening than non-Aboriginal women and are diagnosed with invasive breast cancer at a higher rate than the overall NSW female population.
The project aims to increase participation of Aboriginal and Torres Strait Islander women in routine breast screening. A key element is communications targeting Aboriginal women aged 40–74 in NSW, the Aboriginal health workforce and GPs.
Your assistance to share this information with relevant networks is appreciated.
Note that the recommended screening age for non-Aboriginal women remains 50–74 years.
Thank you for your ongoing support of BreastScreen NSW. Please contact your local BreastScreen NSW service on 13 20 50 for more information.
2022 program news and updates
Own It - ACON to launch a new cervical screening campaign in January

ACON's Own It campaign aims to empower young women and people with a cervix aged 25-35 to make their Cervical Screening Test their own, by choosing how to screen.
The campaign is based on the experiences of real people who have made choices about how their Cervical Screening Test is done, to overcome barriers. Their choices include self-collection, bringing a friend, inserting the speculum themselves, finding a doctor they could trust, talking to others, and educating themselves to address misinformation.
Focus testing found low awareness of the self-collection but when presented as an option there was strong interest. Self-collection has the potential to prompt young women and people with a cervix to screen, including those who are overdue or never screened.
However, testing also highlighted the importance of health services being prepared and willing to provide the self-collection option. Denial of the self-collection option may negatively impact the screening experience and propensity for people to re-test regularly.
Own It will launch on Monday 16 January and run through February. The campaign is inclusive of all people with a cervix regardless of gender, sexuality, cultural background, or ability.
The Own It campaign is part of ACON’s Can We cancer programs brand. It is a partnership with and funded by Cancer Institute NSW.
How primary carers can support the campaign
We encourage you support the campaign by ordering and displaying campaign posters (A3 or A4) for your practice or service. Email: canwe@acon.org.au.
National Cervical Cancer Awareness Week 2022
National Cervical Cancer Awareness Week will be held during the 7-13th November an annual campaign to increase cervical cancer screening rates.
In the very small number of cases where cervical cancer is detected, early diagnosis through screening greatly improves the chances of treatment being successful.
By detecting HPV infection - which usually causes no symptoms - screening identifies women at risk of eventually developing cervical cancer, so they can be monitored and treated accordingly.
The National Cervical Screening Program reduces illness and death from cervical cancer. Women and people with a cervix aged 25 to 74 years of age are invited to have a Cervical Screening Test every 5 years through their healthcare provider.
The National Cervical Screening Program has developed a Healthcare provider toolkit. This toolkit contains resources and information to help healthcare providers engage under-screened people and encourage them to participation in cervical screening. Healthcare providers can print every product and resource in the toolkit.
Cervical screening and female genital mutilation
7-13 November 2022 is Cervical Cancer Awareness Week and a time to reflect on how we can improve our approach to one of the most preventable types of cancer.1
Women who have undergone female genital mutilation/cutting (FGM) have higher levels of cervical cancer2 and human papilloma virus (the main precursor to cervical cancer).3
Female genital mutilation is the practice of partial or complete removal of the external female organs, which is rooted strongly in tradition.4 FGM is internationally recognised as a violation of human rights. It can cause many severe health consequences such as sepsis, chronic pain and infections, infertility, anxiety, post-traumatic stress disorder, and complications in childbirth.
The practice of female genital mutilation is illegal in Australia. Many Australians also migrated from countries that practice FGM, mainly from Africa and the Middle East. However, some women may not be aware that they have undergone FGM, so cervical screening provides an opportunity for FGM to be identified by health care providers.
Cervical screening is an important and sensitive consideration for women who have undergone FGM. There are both barriers and opportunities afforded by the new guidelines around self-collection.
View the NSW Education Program on FGM to learn about providing care to women who have undergone FGM. The NSW Education Program provides a one-day training workshop (with CPD points) for healthcare professionals.
Resources and networks in NSW:
- NSW Education Program on Female Genital Mutilation (FGM) - contact the NSW FGM Program (02) 9840 4182 or (02) 9840 3877
- Family Planning NSW - 1300 658 886
- STARTTS: Service for the Treatment and Rehabilitation of Torture and Trauma Survivors - (02) 9794 1900
FGM is illegal in every state and territory of Australia. This includes sending a person overseas to have a procedure done, or facilitating, supporting or encouraging some to have this done. If you are concerned about the safety of a female baby, a girl or woman who is at risk of female genital mutilation in NSW or being taken out of NSW or Australia for this purpose, you can contact:
- NSW Police - 000
- NSW FGM Program (02) 9840 4182 or (02) 9840 3877
- Child Protection Helpline -132 111
For more information:
Contact Nina Hartcher at Nina.Hartcher@health.nsw.gov.au.
Sources:
1. https://www.iarc.who.int/featured-news/iarc-marks-cervical-cancer-awareness-month-2022/
2. WHO, author. Understanding and addressing violence against women: Female genital mutilation. 2012. [19th June, 2017]. http://apps.who.int/iris/bitstream/10665/77428/1/WHO_RHR_12.41_eng.pdf.
3. Ogah J, Kolawole O, Awelimobor D. High risk human papilloma virus (HPV) common among a cohort of women with female genital mutilation. Afr Health Sci. 2019 Dec;19(4):2985-2992. doi: 10.4314/ahs.v19i4.19. PMID: 32127873; PMCID: PMC7040333.
4. NSW Education Program of Female Genital Mutilation.
Remind women to book a mammogram for Breast Cancer Awareness Month
October is Breast Cancer Awareness Month, an annual campaign to increase screening rates for breast cancer.
According to recent research undertaken by BreastScreen NSW, having a conversation about breast screening is crucial as women aged 50-74 are more likely to get a mammogram if it is recommended by their GPs.
Anthea Temple, BreastScreen NSW Program Manager, is encouraging GPs and Practice Nurses to help boost breast screening numbers, this October “Although a medical referral is not required, we know that GPs and practice nurses have a significant influence on a woman’s decision to screen. You play a central role in supporting and encouraging eligible women to book and attend a breast screening appointment.”
You make a key difference in detecting breast cancer early
Some women are reluctant to have a mammogram. They may be embarrassed about the nature of the procedure or feel anxious about pain or discomfort. By supporting your patients and encouraging eligible women to participate in breast screening, you can make a key difference in a woman’s decision to attend.
For women aged 50-74, a mammogram is the best way to detect breast cancer early, before they or you notice a change. Early detection is the key to improving survival rates, treatment and recovery from breast cancer.
Since the introduction of the BreastScreen program in 1991, there has been a sharp decline in breast cancer-related deaths, due to the combination of earlier detection, and advances in management and treatment.1 Women whose cancers are detected by BreastScreen NSW are less likely to need a mastectomy, compared with women whose breast cancers are found after seeing a doctor to investigate symptoms.2
BreastScreen NSW provides free breast screening for women from 40 years. Women aged 50 – 74 years are invited to screen every two years.
Women can call 13 20 50 to book an appointment or book online.
BreastScreen NSW program is designed for asymptomatic women and not appropriate for the investigation of symptoms. Patients with symptoms should be referred for diagnostic investigation as per the recommended pathway.
Thank you for your support of the BreastScreen NSW program. For more information visit BreastScreen NSW.
For more information, contact:
Trudy Phelps, Relationship Manager, BreastScreen NSW Trudy.Phelps@health.nsw.gov.au
Sources:
[1] 2002, IARC Handbook of Cancer Prevention – Breast Cancer Screening
[2] Australian Government Department of Health and Ageing. Evaluation of the BreastScreen Australia Program — Evaluation Final Report (pages 49–50). Screening Monograph No.1/2009. Canberra: Department of Health and Ageing, June 2009.
‘What is Cancer Screening’ brochure new translations available in 15 languages
The ‘What is Cancer Screening?’ resource, has now been translated into 15 more languages by Multicultural Health Communication Service. This brings the total languages available to 37, with an additional version produced specifically for Aboriginal communities.
The resource explains cervical, breast and bowel screening and what patients should do for each, all in one sheet.
Self-collection now available for cervical screening
A new way for people to take part in the Cervical Screening Test started from 1 July, with self-collection now available to everybody across Australia.
Anyone eligible for a Cervical Screening Test under the NCSP (women and people with a cervix aged 25–74) now has the choice to screen either through self-collection of a vaginal sample using a simple swab (unless a co-test is indicated), or clinician-collection of a sample from the cervix using a speculum.
Pene Manolas, Cervical Screening Program Manager at Cancer Institute NSW, says the new policy has the potential to help more people prevent cervical cancer.
“We know that many people have never screened or are very overdue, and we hope the new collection method could be the encouragement they need to book in,” Ms Manolas explains.
“Self-collection can help breakdown potential barriers of pain or shame and offer empowerment for people to screen themselves.”
Key messages
All participants now have the choice to screen using either a clinician collected sample from the cervix or a self-collected vaginal sample, both accessed through healthcare providers.
HPV testing using self-collected vaginal samples is as accurate as using a clinician-collected sample from the cervix.
Self-collection swab - range of collection devices and methods available to use for self-collection of a vaginal sample for cervical screening. Meaning, different laboratories may have varying collection and handling instructions and requirements. Healthcare providers should contact their local pathology laboratory.
Self-collection must be ordered and overseen by a healthcare provider who can also ensure timely clinician-collection of a cervical sample for liquid-based cytology (LBC) if required as part of a follow-up assessment.
Find out more about self-collection in NSW.
There are a range of resources available on the National Cancer Screening Program website including explainer and instructional videos, information sheets, visual guides, and quick reference guides. Resources are available for:
- general audiences
- Aboriginal and Torres Strait Islander peoples
- culturally and linguistically diverse people
- healthcare providers
Resources | Australian Government Department of Health and Aged Care
NAIDOC Week 2022 Get up! Stand up! Show up!
This year NAIDOC week will be celebrated between 3-10 July.
Get Up! Stand Up! Show Up! Is the theme for NAIDOC week 2022 and supports the importance of narrowing the gap between aspiration and reality, good intent and outcomes.
NAIDOC Week events are held to celebrate and recognise the history, culture and achievements of our First Nations Peoples. The week is a great opportunity to participate in a range of activities and to support your local Aboriginal community.
Between 1998 and 2014 mortality from cancer has increased for Aboriginal people by 21%, while for non-Indigenous people it has decreased by 13%. GPs can play a vital role in prevention and early detection of cancer in Aboriginal people and help stem rising deaths1. This can be achieved by ensuring cancer prevention and screening questions are integrated in Aboriginal Health Checks (715).
Improving cultural safety throughout the cancer pathway for Aboriginal people is a key priority for the Cancer Institute NSW and the Aboriginal Health and Medical Research Council of NSW. This will contribute to “closing the gap” and ensuring better equity of access and outcomes to cancer treatment.
We all have a role to work together in closing the gap and improving outcomes for Aboriginal communities.
Learn more about participation in NAIDOC week events at www.naidoc.org.au/
For more information, contact:
Kathryn Duggan, Primary Care Strategic Advisor, Cancer Institute NSW: cinsw-primarycare@health.nsw.gov.au
Please refer to the Primary Care updates webpage online for previous articles posted - https://www.cancer.nsw.gov.au/what-we-do/working-with-primary-care/primary-care-updates
If you have any queries about this process, please email cinsw-primarycare@health.nsw.gov.au
Sources:
[1] 2002, IARC Handbook of Cancer Prevention – Breast Cancer Screening
[2] Australian Government Department of Health and Ageing. Evaluation of the BreastScreen Australia Program — Evaluation Final Report (pages 49–to50). Screening Monograph No.1/2009. Canberra: Department of Health and Ageing, June 2009.
Bowel Cancer Screening – Take the test out of the drawer and do it

With bowel cancer set to kill more than 1800 people in NSW this year, there is concern that life screening tests could be left sitting in drawers.
The Cancer Institute NSW estimates that between January and June this year more than 100,000 potentially life-saving free bowel cancer screening kits were sent out and have not been returned.
In our communications this month we are highlighting that many people receive the bowel cancer screening test kit in the mail and stick it in a drawer to think about later.
There could be more than 100,000 of these life-saving kits sitting in junk drawers next to old phone chargers and pizza flyers.
We are urging people to get that test out of the drawer and do it.
Bowel cancer is the second biggest cancer killer in NSW. But if it’s found early it can be successfully treated in more than 90 per cent of cases.
The National Bowel Cancer Screening Program sends a bowel cancer screening test kit to all eligible Australians aged 50 to 74, every two years.
The single biggest risk factor for getting bowel cancer is getting older. People in their early 50s have significantly lower screening rates compared to older age groups.
General practitioners can encourage their patients to:
- Do the test when it comes in the mail , don’t put it in the drawer for later
- Order a replacement test from the National Cancer Screening Register (NCSR)
The NCSR enables general practitioners to access view patients screening histories, check their information and order a bowel screening kit. The NCSR is accessible through:
- HealthCare Provider Portal
- Integrated clinical software, Best Practice (Saffron), Medical Director 4.0 and Communicare 21.3
For more information accessing the HealthCare provider portal or the integrated clinical software:
National Cancer Screening Register
For more information on bowel cancer screening visit:
For local data on participation the National Bowel Cancer Screening Program visit:
National Cervical Screening Program Update: Self Collection Policy Change
The self-collection policy will be changing from July 2022. From 1st of July all women and people with a cervix screening under the National Cervical Screening Program (NCSP) will have the choice to screen using either a self-collected vaginal sample or a clinician-collected sample.
Primary health professionals will maintain a central role in consulting with women about the option of self-collection. To support the self-collection policy change, the NCSP: Guidelines for the management of screen-detected abnormalities, screening in specific populations and investigation of abnormal vaginal bleeding have been reviewed and updated.
You can access the updated guidelines on the Cancer Council Australia website or download a PDF version using this link. The partial update to the guidelines has been informed by best available evidence and will come into effect on 1 July 2022.
As cervical screening saves lives, this expanded choice in screening options has the potential to increase participation in cervical screening further.
National Cervical Screening Program resources including fact sheets and education modules will be made available to health professionals in the coming months.
Find out about the Cancer Institute NSW and Royal College of General Practitioners upcoming webinar on self-collection.
Refugee Week – Are we providing the best care we can?
Refugee Week, a national event, is next month, from 19th June to 25th June. In Refugee Week we celebrate the positive contributions of refugees to Australia. Refugee Week also gives us a chance to reflect on how we can provide the best possible healthcare to refugees, including the use of Refugee Health Assessments and interpreters.
Refugee communities have “some of the poorest health outcomes”, according to the NSW Refugee Health Service. Refugees and asylum seekers have often experienced persecution, violation of human rights, and deprivation and disruption of basic healthcare.
General practitioners can access Refugee Health Assessments to conduct post-arrival health assessment of people from a refugee background which can be covered under Medicare. In Australia, refugees and other immigrants experience dramatic disparities in cancer screening. Health professionals should recognise the barriers to health-seeking behaviours among refugee populations such as cultural influences and poor knowledge of health services and health systems. It is important that general practitioners identify gaps in a patients’ health care and tailor their healthcare approach to refugees.
General practitioners can use interpreters to communicate with patients who are not fluent in English. To gain priority access to the Translating and Interpreting Service (TIS), medical practitioners and allied health professionals can register for the Doctors Priority Line here.
Refugees provide a rich diversity to Australian culture, and with this diversity comes diverse healthcare needs, which we can all consider to improve our practice for refugee communities.
Need Help?
- For more information on primary care for people with a refugee background, visit the NSW Refugee Health Service website
- For support on using interpreters, you can view the practical guide called “Engaging Interpreters in Cancer Settings” in the Cancer Institute NSW’s primary care toolkit.
Quick stats
- At the end of 2020, 82.4 million people were forcibly displaced globally
- Australia’s Humanitarian Program grants 13,750 visas per year to refugees and asylum seekers. This was reduced from 18,750 in 2020.
- Due to COVID-19, only 5974 visas were granted in 2020-2021.
Quick Stats: Refugees in NSW 2015-2020
- 30,000 humanitarian visas
- Most common countries: Syria, Iraq, Afghanistan, Democratic Republic of Congo, Myanmar
- 92% had poor or no English proficiency
- ¼ were children under 11 years
For more information, contact:
Nina Hartcher – Project Officer: Nina.Hartcher@health.nsw.gov.au
Integration of The National Cancer Screening Register with GP practice software
Primary health care providers are important partners in the promotion and delivery of cancer screening programs. Understanding your patient population and who is participating in the National cervical and bowel screening programs, is vital in enhancing participation.
The National Cancer Screening Register (NCSR) is now integrated with most clinical information systems to enable healthcare providers to access and report clinical data for the National Cancer Screening Register from existing clinical information systems, including Best Practice Saffron (Jan 2021), Medical Director 4.0 (Aug 2021) and Communicare (Dec 2021).
Healthcare providers who integrate their Clinical Information System with the NCSR have better access to screening histories for their patients and can interact with the NCSR directly. To integrate the NSCR with GP practice software, practices are required to complete one linkage for authentication via PRODA account. Once integration is complete, the practice will have access to all the functionalities of the healthcare provider portal whilst working within their practice management system.
Need Help?
GP practices can access support from an NCSR specialist. Book your walk through with an NCSR specialist using this link. Please don’t delay the NCSR are there to help.
Visit Cancer Screening and Primary Care for information and resources to support enhancement in cancer screening for your community.
For more information, contact:
Kath Duggan – Primary Care Strategic Advisor Kathryn.Duggan@health.nsw.gov.au
Report shows Cervical screening rates need to improve
In December 2021 the Australian Institute of Health and Welfare (AIHW) released the National Cancer Screening Program Monitoring Report1 inclusive of data captured for women aged 25-74 screened under the renewed 5-year program.
Whilst participation in the new 5-year program cannot properly be reported until 5 years of data is available, preliminary estimates have demonstrated that there is a significant level of under screened women both nationally and at the NSW state level.
For the first 3 years, 2018-2020 the national cervical screening participation rate was 56% for women aged between 25 and 74. NSW was below the national average with a participation rate of 54%. This leaves 46% of women aged between 25-74 overdue for cervical screening and at risk of delayed Human Papillomavirus (HPV) detection.
There is a demonstrated need to increase cervical screening participation within NSW to reduce preventable cervical cancer incidence and mortality. As the frontline of healthcare, primary care professionals have a critical role in both providing women with cervical screening and empowering their patients with knowledge about the benefits of screening. Actively engaging with your overdue patients in a conversation about cervical screening will have a significant impact on increasing participation rates. Here is some information on how to support patients in cervical screening.
ALERT: Cervical screening self-collection policy will be changing from July 2022
From 1 July 2022, the National Cervical Screening Program (NCSP) will expand screening test options, offering self-collection as a choice to all people participating in cervical screening. Recent evidence2 demonstrates a Cervical Screening Test using a self-collected vaginal sample is as accurate as a clinician-collected sample taken from the cervix during a speculum examination. Primary health professionals will maintain a central role in consulting with women about the option of self-collection and facilitating the self-collection pathway.
More information to follow in the April Primary Care Update.
For any queries, please contact Teresa Fisher, Relationship Manager Cervical Screening: teresa.fisher@health.nsw.gov.au
1. Australian Institute of Health and Welfare 2021. National Cervical Screening Program monitoring report 2021. Cancer series 134. Cat. no. CAN 141. Canberra: AIHW.
2. Arbyn, M., et al., Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: updated meta-analyses. BMJ, 2018. 363: p. k4823
Announcing the Refugee Cancer Screening Partnership Project
Harmony Day, on Monday 21st March this year, celebrates Australia’s cultural diversity and encourages respect and inclusiveness for all Australians, including those from refugee and migrant communities. More information can be found on the Australian Government website. Cancer Institute NSW is delighted to announce the commencement of the Refugee Cancer Screening Partnership Project, which will focus on improving the inclusion of Middle Eastern and Sub-Saharan refugee communities in Australia’s national cancer screening programs.
Cancer Institute NSW, along with partner agencies NSW Refugee Health Service and Settlement Council of Australia, is leading a multi-agency partnership project that aims to create awareness and improve participation of Middle Eastern and Sub-Saharan refugee communities in Cervical, Breast, and Bowel Cancer Screening Programs. Settlement agencies from across NSW will be engaged to work with local communities, including STARTTS, Illawarra Multicultural Services, Northern Settlement Services and Metro Assist Inc.
As Primary health care providers are essential partners in cancer screening, this project will involve Primary Health Networks, Medical Associations and primary health care providers in the governance of this project. The findings will be promoted on a national level to improve our understanding of best practice for cancer screening in refugee communities.
For more information, please contact Nina Hartcher: Nina.Hartcher@health.nsw.gov.au
Primary Care and National Close the Gap Day
National Close the Gap Day will be observed on Thursday 17 March this year. The Close the Gap campaign advocates for health equity of Australia’s indigenous people and educates the public about the health issues and barriers to well-being faced by them.
The campaign is aimed at improving the health outcomes of Aboriginal and Torres Strait Islander people, whose life expectancy is 10–17 years lower than that of non-indigenous Australians. In addition to access to healthcare, other factors including poverty, education, and employment have an impact on the well-being of indigenous groups.
Actions must be taken in all of these areas to raise the standard of living for indigenous people and close the gap in healthcare and access to health resources.
Close the Gap advocates for health care choice and access, a responsive healthcare system that is sensitive to cultural and linguistic differences, and safe housing that promotes good health.
Primary Care can help reduce cancer rates in Aboriginal and Torres Strait Islander population.
Between 1998 and 2014 mortality from cancer has increased for Indigenous people by 21%, while for non-Indigenous people it has decreased by 13%. GPs can play a vital role in prevention and early detection of cancer in Aboriginal and Torres Strait Island people and help stem rising deaths1.
Improving culturally appropriate and safe cancer support throughout the cancer pathway for Aboriginal people is a key priority for Cancer Institute NSW (the Institute) and the Aboriginal Health and Medical Research Council of NSW (AH&MRC) and the contributing to “closing the gap” and better equity of access and outcomes in regard to cancer treatment.
In NSW approximately 50% of Aboriginal and Torres Strait Islander people access Indigenous-specific primary health care services, with the other 50% access general primary health care services2. Asking all your clients about Indigenous status is particularly important as GPs have a very important role to play in prevention and early detection of cancer.
Aboriginal and Torres Strait Islander health checks (715-health check) ensure that Indigenous Australians receive primary health care matched to their needs. The 715-health check encourages early detection, diagnosis and intervention for chronic disease, including cancer, that causes morbidity and early death. Incorporating cancer screening into these checks is an excellent way to lift cancer screening participation rates among people who may have an increased risk of cancer due to age and/or lifestyle risk factors.
HOW TO PARTICIPATE IN NATIONAL CLOSE THE GAP DAY
1. People often have inequitable access to health resources, making them more susceptible to disease and poor health outcomes. Identify clients who are most at risk and how you can help support programs that improve healthcare
- Promote cancer screening participation - access resources
- Promote quit smoking - access resources
2. RACGP has developed a useful resource for general practices to improve their identification processes of Aboriginal and Torres Strait Islander people. You can access resources online here.
3. Ensure your Primary Care team has undertaken cultural awareness and cultural safety training. Read the RACGP’s Cultural awareness training and cultural safety training guidelines for more information on training options
4. Take the opportunity to audit your client records and recall those identified to be of Aboriginal and/or Torres Strait Islander descent and extend an invitation to complete an Aboriginal health check (715) if due or overdue. Take this opportunity to promote participation in cancer screening and lifestyle modification actions such as quit smoking.
For more information, contact Alisha McInerney: alisha.mcinerney@health.nsw.gov.au
1. GPs can help reduce cancer rates in Aboriginal and Torres Strait Islander population https://www1.racgp.org.au/newsgp/clinical/gps-can-help-reduce-high-rates-of-cancer-in-aborig
2. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19 https://www.indigenoushpf.gov.au/measures/3-17-regular-gp-health-service
Bowel Cancer Screening campaign relaunch
Primary health care providers are important partners in the promotion and delivery of cancer screening programs. Research shows that a primary health care provider recommending or endorsing bowel cancer screening increases participation in the National Bowel Cancer Screening Program.
The campaign was launched in 2021 featuring Dr. Norman Swan encouraging people aged 50-74 to Do the Test when it arrives in the mail, as if detected early, bowel cancer can be successfully treated in more than 90% of cases.
This year the campaign will run from 6 February to 28 May 2022, and be expanded to include out of home advertising and some additional social media content.
Discover more about the new ‘Do the test’ campaign HERE

An important message about BreastScreen NSW
The BreastScreen NSW service is open. Some services are affected by the impact of COVID-19 on staffing and the need to redeploy staff to support the local pandemic response.
BreastScreen North Coast which services Northern NSW and Mid North Coast Local Health Districts (LHD), has temporarily closed screening sites at Coffs Harbour, Lismore, Port Macquarie and Tweed Heads, and mobile van screening locations in the region. Clients will be contacted about any change to appointments.
All other services are currently operating.
If you have any questions about appointments or the availability of your local service, please call 13 20 50 or for further information please visit BreastScreen NSW's website.