Information about accessing and referring for colonoscopy in NSW
There are three main pathways for a patient to access a colonoscopy in NSW. The pathway they take will affect:
- how they are assessed prior to the procedure (in person or over the phone)
- the out-of-pocket costs associated with the pre-colonoscopy assessment and the colonoscopy itself
- the time they will need to wait to have their colonoscopy.
Following a positive bowel screening result, a patient will be referred to:
- The Direct Access Colonoscopy (DAC) service of a public hospital: Most patients will be assessed over the phone prior to the day of the colonoscopy. There will be no out-of-pocket costs to the patient for either the pre-colonoscopy consultation or the procedure itself. More details below.
- The outpatient gastroenterology clinic of a public hospital: The patient will need to attend the hospital in person to be assessed prior to the day of the colonoscopy. There will be no out-of-pocket costs to the patient for the pre-colonoscopy consultation or the procedure itself if the colonoscopy is then done in a public hospital.
- A private specialist’s (gastroenterologist or colorectal surgeon) rooms: The patient will typically need to be seen in person to be assessed prior to the colonoscopy which often incurs an out-of-pocket cost.
It is important for patients to be fully informed of the options available to them. They should also be informed of financial or other implications prior to being referred. Find information on facilitating informed financial consent.
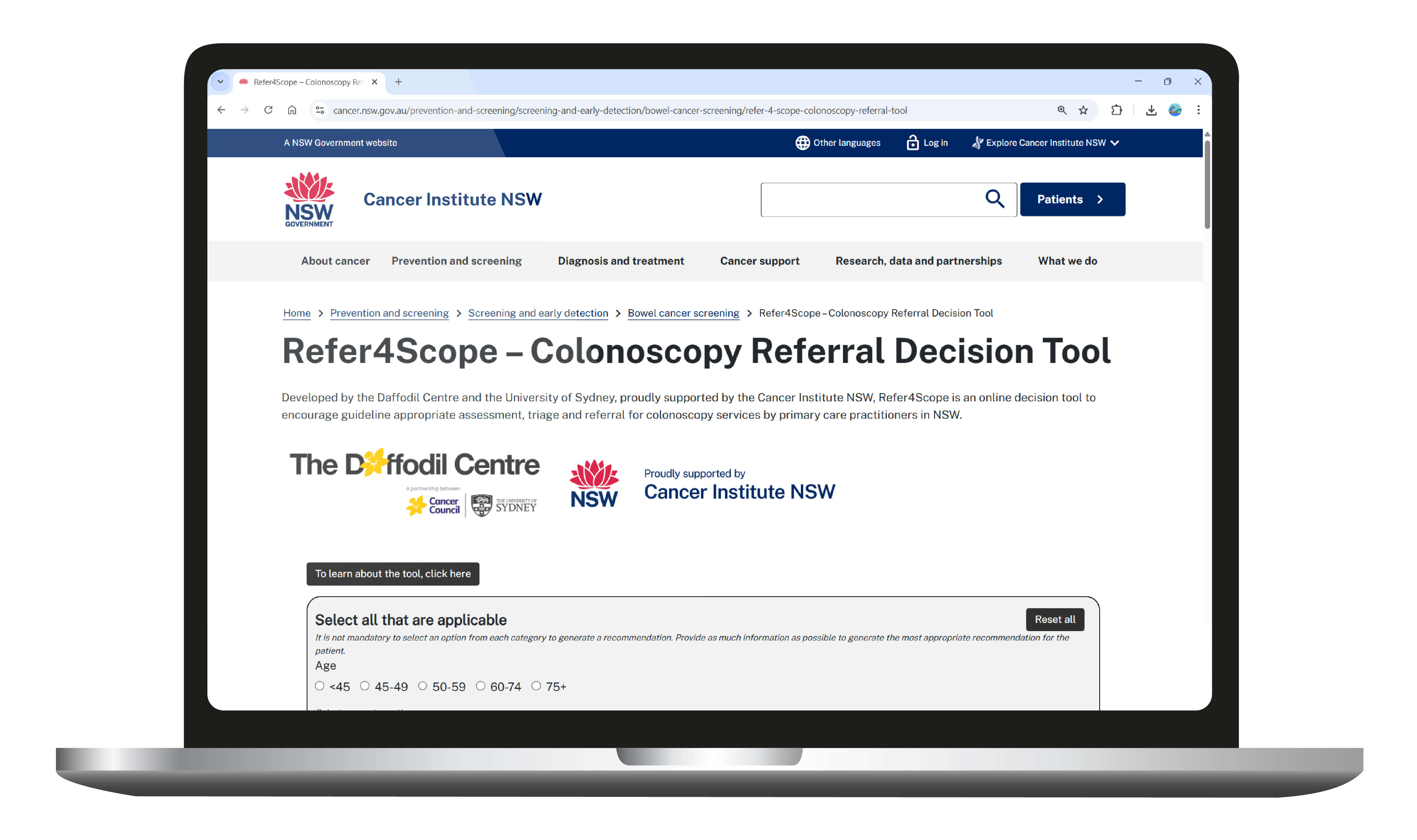
Refer4Scope, co-designed by the University of Sydney and the Daffodil Centre, is a decision tool for primary health care providers to support clinical assessment and referral of patients requiring a colonoscopy based on a colorectal cancer screening result, bowel-related symptoms and/or family history of colorectal cancer.
During a patient consult, primary health care providers can follow the quick and easy prompts to input their patient’s information and receive clinically-accurate recommendations in moments.
Refer4Scope was developed by leading experts and co-designed with clinicians. It draws from the 2023 update to the 'Clinical Practice Guidelines for the prevention, early detection and management of colorectal cancer'.
View a short video tutorial on how to use the Refer4Scope tool (1.45 mins) below.
The following short videos are from the ‘Colonoscopy referral education for primary care webinar’, presented in June 2025.
This webinar was aimed at supporting primary health care providers with guideline appropriate assessment, triage and referral for colonoscopy services in NSW.
The webinar was presented by:
- A/Prof Eleonora Feletto, Cancer Elimination Centre, Sydney School of Public Health, University of Sydney
- Dr Cameron Bell AM, Director of Endoscopy and Senior Staff Specialist at Royal North Shore Hospital
- Mr Christopher Horn, Head of the NSW Bowel Screening Program at Cancer Institute NSW
This webinar was accredited by the Royal College of General Practitioners (RACGP) and the Australian College of Rural and Remote Medicine (ACRRM).
Educational videos
Educational Video 1: Colorectal Cancer Risk and Screening Pathways (8.16 mins)
Educational Video 2: Colonoscopy Services in NSW (8.04 mins)
Educational Video 3: Colonoscopy Referral and Patient Interaction (7.27 mins)
Patient case study videos
In these videos, patient case studies are used to demonstrate the:
- Triage process – using the clinical guidelines and Refer4Scope decision tool to support clinical decision-making
- Referral process – available colonoscopy referral options in NSW and other factors to consider in making a referral
Case study 1: Family history of colorectal cancer (7.41 mins)
Case Study 2 : Negative iFOBT with bowel symptoms (6.55 mins)
Case Study 3 : Positive iFOBT (7.45 mins)
For all colonoscopy referrals, it is crucial that primary health care providers include sufficient information for the receiving clinician to assess the appropriateness, risk and urgency of consultation. Comprehensive referrals prevent delays and allow accurate assessment of the patient’s suitability for colonoscopy and for DAC.
“Referral documentation greases the wheels of the whole process and can hinder or help streamlined access to colonoscopy and streamlined decision making about whether a colonoscopy is indicated”. Gastroenterologist in NSW
While each DAC service has their own clinical criteria specific to their local circumstances (see HealthPathways links in the table below), in general, colonoscopy referrals should include the following information:
- Indication for the referral including bowel symptoms, iFOBT results and/or family history of colorectal cancer (including age of diagnosis of first-degree relatives).
- Relevant medical history, including cardiorespiratory disease, diabetes, abdominal and pelvic surgery.
- Current medicines including anti-coagulants, diabetic and weight loss medications.
- Results of previous investigations, including iFOBT (indicating whether this was through the NBCSP), colonoscopies, histopathology and other recent pathology. Note: Recent blood testing results should be limited to what's relevant to the decision about colonoscopy (FBC, EUC, LFT, iron studies).
For more information see:
- Australian Commission on Safety and Quality in Health Care fact sheet outlining key components of a comprehensive referral
- NSW Health state-wide referral criteria - Concern for colorectal cancer (rectal bleeding or positive Faecal Occult Blood Test)
- Refer4Scope – Colonoscopy Referral Decision Tool
- Colonoscopy Referral Education Videos for Primary Care
- National Bowel Cancer Screening Program Colonoscopy referral checklist (PDF)
- Clinical practice guidelines for the prevention, early detection and management of colorectal cancer
- Colonoscopy Clinical Care Standard | Australian Commission on Safety and Quality in Health Care
- NSW colonoscopy categorisation I Agency for Clinical Innovation

Information about Direct Access Colonoscopy
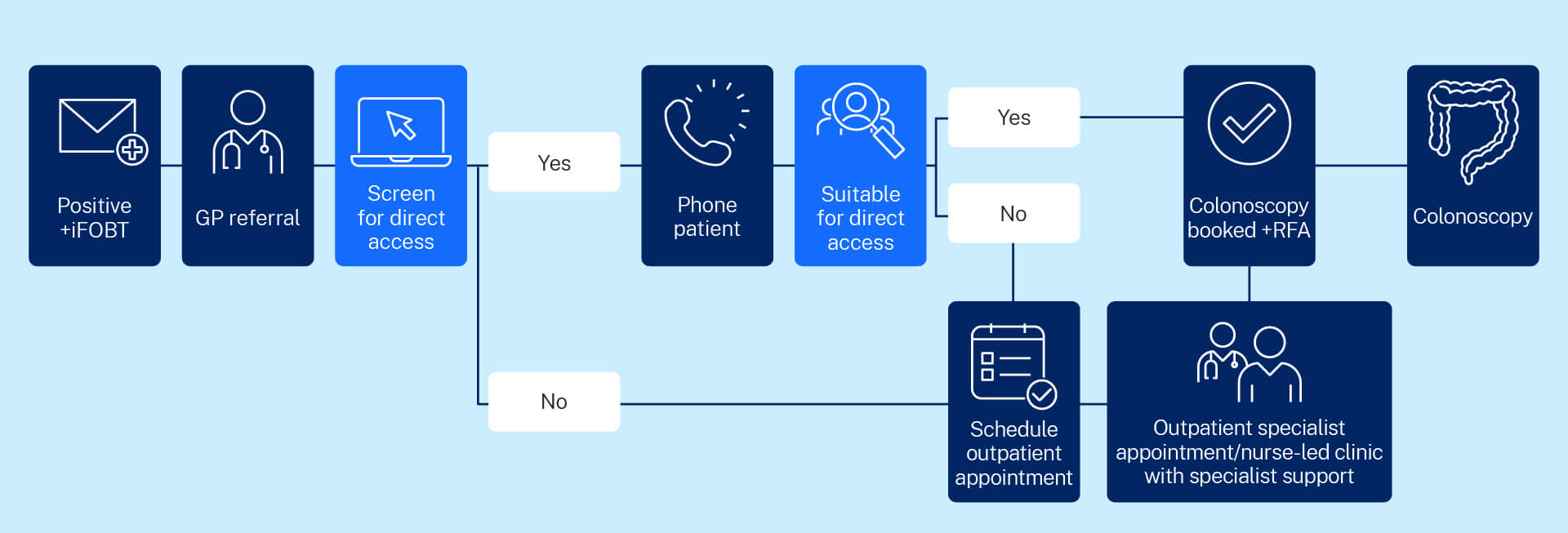
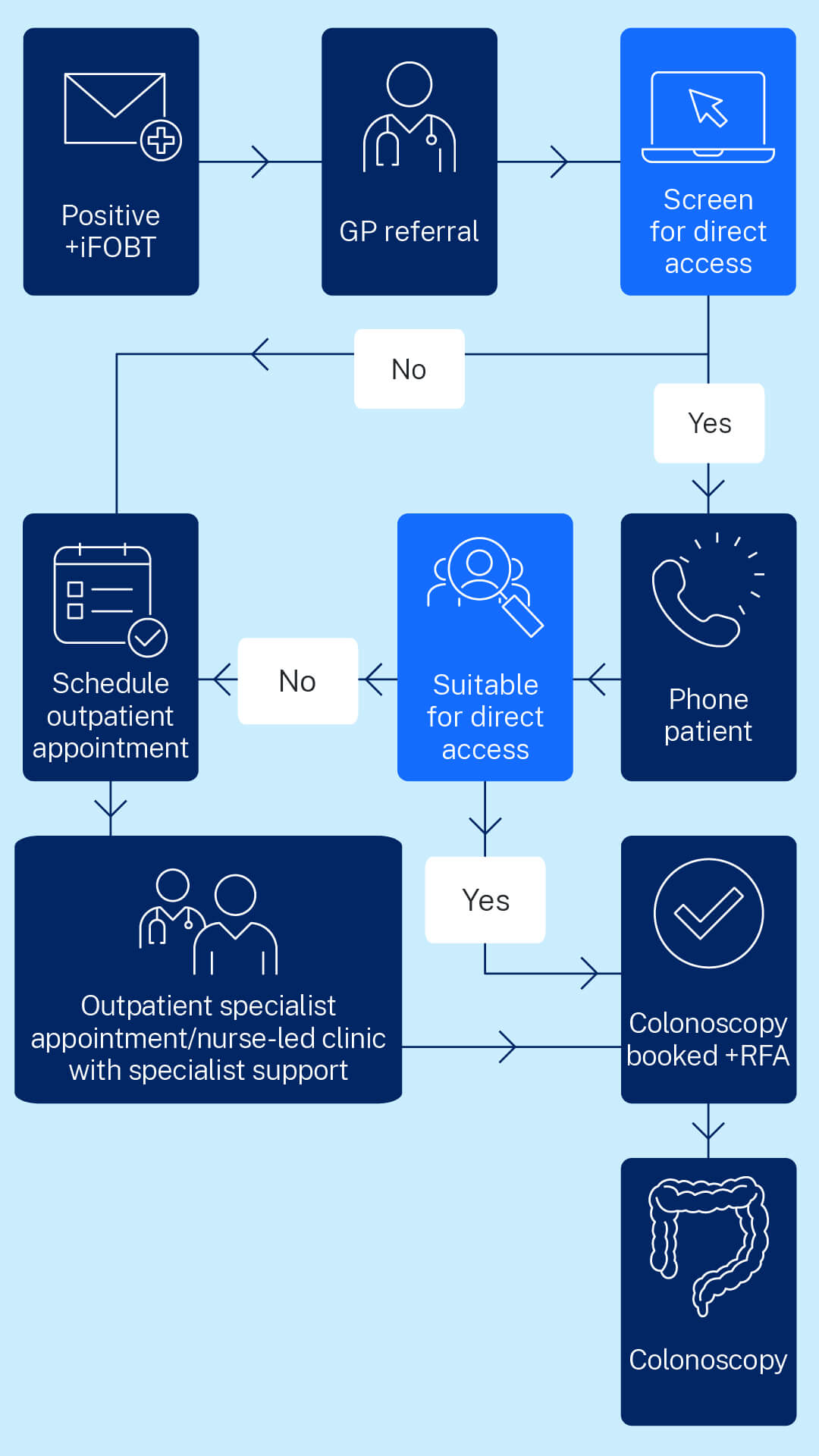
DAC is a NSW Health value based health care initiative that focuses on helping people gain access to public colonoscopy services after a positive bowel cancer screening test.
A key advantage of DAC is that it allows otherwise healthy patients who have a positive iFOBT and meet the inclusion criteria, to be assessed and triaged during a free telephone appointment with a specially trained nurse.
This is an alternative to having a face-to-face appointment with a specialist prior to the day of the colonoscopy. A nurse-led telephone triage assessment enables patients to be referred directly to a DAC service.
If patients are suitable for telephone assessment, they will only need to come to the hospital once on the day of their procedure.
DAC services improve access to colonoscopy for people in NSW by reducing barriers commonly faced by patients such as:
- Extended wait times for clinic appointments
- Unnecessary face to face appointments
- The need to take time off work
- Time spent travelling to specialists/outpatient appointments
- Out-of-pocket costs for private specialist room appointments
- Anxiety and psychological distress (exacerbated by lengthy waiting periods)
Other benefits of DAC services are that they:
- Improve access to public colonoscopy, especially in areas without an existing outpatient clinic
- Free up clinic time for patients with more complex issues (by redirecting patients who do not need to be seen in person to a DAC telephone assessment)
- May contribute to earlier detection of bowel cancer which can lead to reduced morbidity and mortality for patients
- Have a well-structured and protocolised triage and assessment pathway which assures safe, independent assessment by nursing staff with specialist oversight
They will need to make a face-to-face appointment in clinic or private rooms with a specialist before their colonoscopy.
The DAC model of care outlines the mandatory and recommended inclusions for implementation and should be read in conjunction with the following:
- the Australian Commission on Safety and Quality in Health Care Colonoscopy Clinical Care Standard 2025
- the National Safety and Quality Health Service Standards
- the National Health and Medical Research Council (NHMRC) Clinical Practice Guidelines for Surveillance Colonoscopy
- Local Health District (LHD) and Speciality Hospital Networks (SHN) policies and procedures.
In 2024, the model of care was revised to ensure accuracy and to incorporate any changes to practice since the model was first published in 2020.
Each DAC service have their own clinical criteria specific to their local circumstances, however, in general the referral criteria require a patient aged 45-75 years to have returned a positive iFOBT, be asymptomatic and otherwise healthy.
For more information on eligibility, consider using Refer4Scope, an online decision tool to support assessment, triage, and referral for colonoscopy services by primary health care providers.
Refer to the section below to be directed to your local HealthPathways colonoscopy information page for local eligibility criteria.
Refer to the table below to be directed to your local HealthPathways colonoscopy information page for local referral information and forms. If you do not use HealthPathways, please refer to the ‘alternative referral contact details’ column.
As DAC is a value based health care initiative, in 2024, the Cancer Institute NSW conducted an outcome evaluation of the statewide implementation of DAC services, including:
- Analysis of linked administrative data
- Economic evaluation
- Surveys and interviews with clinicians
- Patient-reported experience measures (PREM) survey
The DAC outcome evaluation report will be released late-2025.
GP DAC information flyer - Fast-tracking your patient to colonoscopy (PDF)
Participant DAC information flyer - Following up on your positive result (PDF)
Direct Access Colonoscopy service locations and referral information
There are several established DAC and other expedited public colonoscopy services available across NSW. Most Local Health Districts (LHDs) have at least one operational DAC service. Please see the map or service directory drop downs below to find your nearest available DAC service.
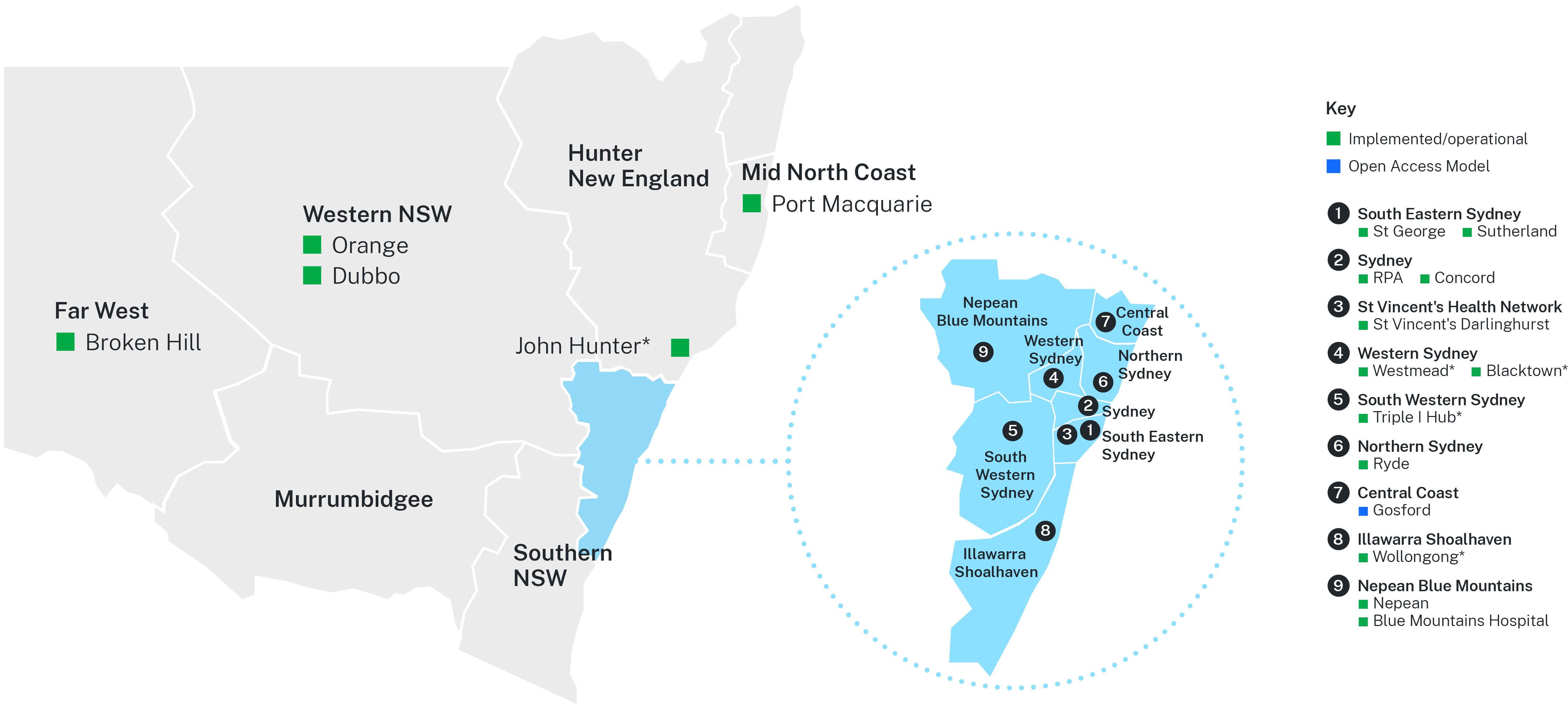
*These services book to a number of hospitals in their region. See full list of hospitals below.
Service directory
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Royal Prince Alfred Hospital (RPAH) Concord Repatriation Hospital | RPAH DAC Service: Phone: 0439 653 371 Fax (02) 9515 8242 Level 9 Concord Hospital DAC Service: Phone: (02) 9767 5570 Fax: (02) 9767 6767 |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
St Vincent’s Hospital Darlinghurst | Referral information/criteria (Sydney HealthPathways) Referral information/criteria (South Eastern Sydney HealthPathways) | St Vincent’s Hospital DAC Service: Phone: (02) 8382 2380 Fax: (02)8382 3983 Level 2, Xavier Building Referral form (Sydney) Referral form (South Eastern Sydney) |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
St George Hospital Sutherland Hospital St Vincent’s Hospital Darlinghurst | St George Hospital DAC Service: SESLHD-StGeorge-GastroLiver@health.nsw.gov.au 1st floor, Burt Neilsen Wing HealthLink SmartForm e-referrals preferred at St George Sutherland Hospital DAC Service: Fax: (02) 9540 8754 Email: seslhd-sutherland-gastroclinic@health.nsw.gov.au Perioperative and Gastroenterology Clinic, Level 3 |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Ryde Hospital Accepts patients from across Northern Sydney LHD | Ryde Hospital DAC Clinic: Phone: (02) 9858 7174 or 0474 013 823 (Tues, Thursday, Friday) Email: NSLHD-Ryde-DAC@health.nsw.gov.au Note: Only HealthLink Electronic referrals (eReferral) accepted. |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Triple I Hub: This service books to:
| Triple I Referral form | Triple I Hub: Phone: 1800 455 511 Fax (02) 4621 8799 |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Blacktown Hospital Also books to:
Westmead Hospital Also books to:
| Referral information/criteria (see ‘Subspecialty clinics’ section) | Blacktown Rapid Access FOBT Clinic: Westmead Rapid Access FOBT Clinic: Fax: (02) 8890 5118 Email: WSLHD-Westmead-FOBT@health.nsw.gov.au |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Blue Mountains Hospital Nepean Hospital |
| Blue Mountains DAC Clinic: Nepean DAC Service: |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
John Hunter Hospital (JHH) Also books to: Other hospitals in the Lower Hunter region. | John Hunter Hospital DAC Service: SeNT eReferral (preferred) |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Wollongong Hospital Also books to: Shellharbour Hospital | Wollongong Hospital Gastroenterology: Phone: (02) 4222 5180 Fax: (02) 4222 5170 |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Port Macquarie Base Hospital Also books to:
| Port Macquarie DAC Service Email: Belinda.Garvey@health.nsw.gov.au |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
Orange Health Service Also books to:
Dubbo Health Service | Orange Health Service DAC Clinic: Email: WNSWLHD-OrangeDACprogram@health.nsw.gov.au Fax: (02) 6369 2360 Dubbo Health Service DAC Clinic: Email: Frances.Obrien1@health.nsw.gov.au Dubbo Health Service utilises eReferrals |
| Hospitals | HealthPathways | Alternative referral contact details |
|---|---|---|
| Broken Hill Hospital | Broken Hill Base Hospital DAC Clinic: Email: FWLHD-DACC@health.nsw.gov.au Broken Hill Base Hospital utilises eReferrals |